 “Chronic pain can be recurrent or constant pain that lasts for longer than 3 months and can result in disability, suffering, and a physical disturbance. Related to the complex nature of chronic pain, treatments have a pharmacological and non-pharmacological approach.
“Chronic pain can be recurrent or constant pain that lasts for longer than 3 months and can result in disability, suffering, and a physical disturbance. Related to the complex nature of chronic pain, treatments have a pharmacological and non-pharmacological approach.
Due to the opioid epidemic, alternative therapies have been introduced, and components of the plant Cannabis Sativa, Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) have gained recent interest as a choice of treatment.
The current pharmaceutical products for the treatment of chronic pain are known as nabiximols, and they contain a ratio of THC combined with CBD, which has been promising.
This review focuses on the treatment efficacy of CBD, THC: CBD-based treatments for chronic pain and adverse events with each.”
https://pubmed.ncbi.nlm.nih.gov/33004159/
https://www.sciencedirect.com/science/article/pii/S1521689620300458?via%3Dihub

 “Fish oil (FO) and phytocannabinoids have received considerable attention for their intestinal anti-inflammatory effects.
“Fish oil (FO) and phytocannabinoids have received considerable attention for their intestinal anti-inflammatory effects. “Cannabidiol (CBD) is known for its vasorelaxant (including in the human pulmonary artery), anti-proliferative and anti-inflammatory properties. The aim of our study was to examine the potential preventive effect of chronic CBD administration (10 mg/kg/day for three weeks) on monocrotaline (MCT)-induced pulmonary hypertension (PH) rats.
“Cannabidiol (CBD) is known for its vasorelaxant (including in the human pulmonary artery), anti-proliferative and anti-inflammatory properties. The aim of our study was to examine the potential preventive effect of chronic CBD administration (10 mg/kg/day for three weeks) on monocrotaline (MCT)-induced pulmonary hypertension (PH) rats.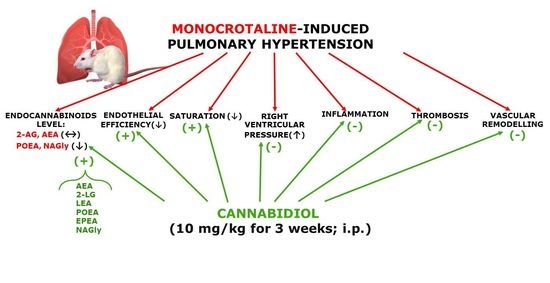
 “Pancreatic cancer (PC) is related to lifestyle risks, chronic inflammation, and germline mutations in BRCA1/2, ATM, MLH1, TP53, or CDKN2A. Surgical resection and adjuvant chemotherapy are the main therapeutic strategies but are less effective in patients with high-grade tumors.
“Pancreatic cancer (PC) is related to lifestyle risks, chronic inflammation, and germline mutations in BRCA1/2, ATM, MLH1, TP53, or CDKN2A. Surgical resection and adjuvant chemotherapy are the main therapeutic strategies but are less effective in patients with high-grade tumors.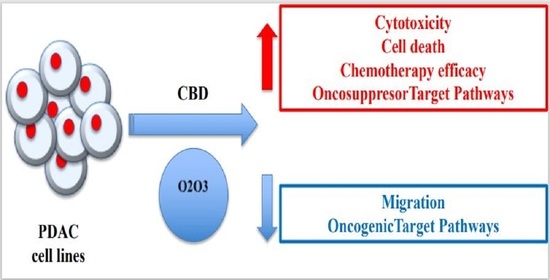
 “In recent years there has been a growing appreciation by regulatory authorities that cannabis-based medicines can play a useful role in disease therapy.
“In recent years there has been a growing appreciation by regulatory authorities that cannabis-based medicines can play a useful role in disease therapy. “Cannabidiol (CBD) is reported to produce pain relief, but the clinically relevant cellular and molecular mechanisms remain uncertain.
“Cannabidiol (CBD) is reported to produce pain relief, but the clinically relevant cellular and molecular mechanisms remain uncertain.