“HER2 (human epidermal growth factor receptor 2) is a well-established oncogenic driver and therapeutic target in breast cancer.
Cannabidiol (CBD), a non-psychoactive phytocannabinoid, has demonstrated anticancer potential, yet its mechanisms of action in HER2-positive breast cancer remain insufficiently characterized.
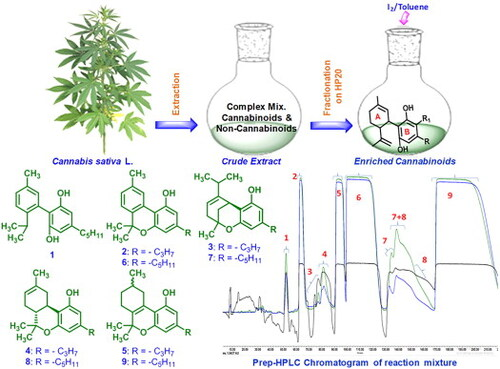
In this study, we examined the effects of CBD on HER2-positive (SK-BR-3, BT-474) and HER2-negative (MCF-7, MDA-MB-231) breast cancer cell lines, with a focus on its interaction with HER2.
CBD selectively reduced the viability of HER2-positive cells, an effect associated with increased intracellular reactive oxygen species (ROS) and a marked reduction in HER2 protein levels. Mechanistically, CBD triggered non-apoptotic cell death pathways, including paraptosis and ferroptosis, as indicated by the modulation of specific molecular markers such as reduced Alix and elevated ATF4 and CHOP for paraptosis, and downregulated GPX4 and SLC7A11 with upregulated TFRC for ferroptosis. HER2 knockdown attenuated CBD-induced cytotoxicity, while HER2 overexpression sensitized cells to CBD, underscoring the HER2-dependence of these effects. Molecular docking predicts the binding conformation and key interactions of ligand with target proteins providing initial insights into potential molecular recognition. Subsequently, molecular dynamics simulations extend this analysis by assessing the stability, flexibility, and energetic characteristics of the ligand-protein complex within a dynamic biological environment.
These findings support a model in which CBD downregulates HER2 and, in a HER2-dependent context, promotes paraptosis and ferroptosis. In addition, docking and molecular dynamics analyses suggested a potential interaction between CBD and HER2, providing mechanistic insights into possible molecular recognition relevant to HER2-positive breast cancer.”
https://pubmed.ncbi.nlm.nih.gov/41621547
“These results suggest that CBD targets HER2, offering a new therapeutic strategy for HER2-positive breast cancer management.”
https://www.sciencedirect.com/science/article/abs/pii/S0925443926000256?via%3Dihub