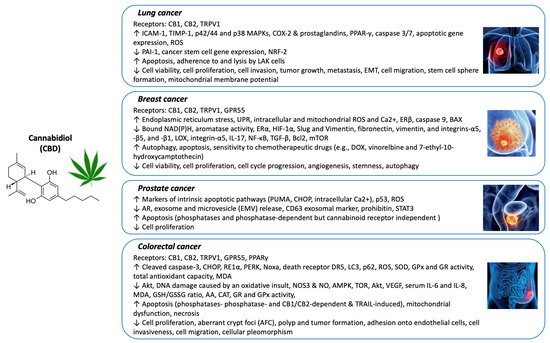
“Introduction: Several studies have shown anti-tumor effects of components present in cannabis in different models. Unfortunately, little is known about the potential anti-tumoral effects of most compounds present in cannabis in bladder cancer and how these compounds could potentially positively or negatively impact the actions of chemotherapeutic agents. Our study aims to evaluate the effects of a compound found in Cannabis sativa that has not been extensively studied to date, cannflavin A, in bladder cancer cell lines. We aimed to identify whether cannflavin A co-treatment with agents commonly used to treat bladder cancer, such as gemcitabine and cisplatin, is able to produce synergistic effects. We also evaluated whether co-treatment of cannflavin A with various cannabinoids could produce synergistic effects.
Results: Cell viability of bladder cancer cell lines was affected in a concentration-dependent fashion in response to cannflavin A, and its combination with gemcitabine or cisplatin induced differential responses-from antagonistic to additive-and synergism was also observed in some instances, depending on the concentrations and drugs used. Cannflavin A also activated apoptosis via caspase 3 cleavage and was able to reduce invasion by 50%. Interestingly, cannflavin A displayed synergistic properties with other cannabinoids like Δ9-tetrahydrocannabinol, cannabidiol, cannabichromene, and cannabivarin in the bladder cancer cell lines.
Discussion: Our results indicate that compounds from Cannabis sativa other than cannabinoids, like the flavonoid cannflavin A, can be cytotoxic to human bladder transitional carcinoma cells and that this compound can exert synergistic effects when combined with other agents. In vivo studies will be needed to confirm the activity of cannflavin A as a potential agent for bladder cancer treatment.”
https://pubmed.ncbi.nlm.nih.gov/35869542/
“A study recently demonstrated that the combination of Δ9-tetrahydrocannabinol and cannabichromene produced synergistic effects in a bladder cancer model, while another focused on the effects of cannabidiol and their potential formulation within nanoparticles to treat bladder cancer. Here, we show that other compounds from cannabis, like cannflavin A, may also induce beneficial cytotoxic and synergistic effects on bladder cancer cells. Our results also showed the ability of cannabinoids, other than Δ9-tetrahydrocannabinol, to produce synergistic effects when combined with the flavonoid cannflavin A.”
https://jcannabisresearch.biomedcentral.com/articles/10.1186/s42238-022-00151-y