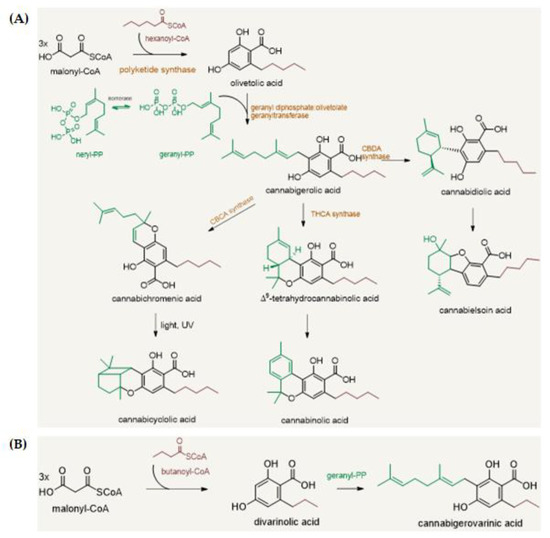
“Cannabis sativa L. is a source of over 150 active compounds known as phytocannabinoids that are receiving renewed interest due to their diverse pharmacologic activities. Indeed, phytocannabinoids mimic the endogenous bioactive endocannabinoids effects through activation of CB1 and CB2 receptors widely described in the central nervous system and peripheral tissues.
“Cannabis sativa L. is a source of over 150 active compounds known as phytocannabinoids that are receiving renewed interest due to their diverse pharmacologic activities. Indeed, phytocannabinoids mimic the endogenous bioactive endocannabinoids effects through activation of CB1 and CB2 receptors widely described in the central nervous system and peripheral tissues.
All phytocannabinoids have been studied for their protective actions towards different biological mechanisms, including inflammation, immune response, oxidative stress that, altogether, result in an inhibitory activity against the carcinogenesis.
The role of the endocannabinoid system is not yet completely clear in cancer, but several studies indicate that cannabinoid receptors and endogenous ligands are overexpressed in different tumor tissues.
Recently, in vitro and in vivo evidence support the effectiveness of phytocannabinoids against various cancer types, in terms of proliferation, metastasis, and angiogenesis, actions partially due to their ability to regulate signaling pathways critical for cell growth and survival.
The aim of this review was to report the current knowledge about the action of phytocannabinoids from Cannabis sativa L. against cancer initiation and progression with a specific regard to brain, breast, colorectal, and lung cancer as well as their possible use in the therapies. We will also report the known molecular mechanisms responsible for such positive effects.
Finally, we will describe the actual therapeutic options for Cannabis sativa L. and the ongoing clinical trials.”
https://www.mdpi.com/1420-3049/26/9/2668

 “The therapeutic potential of
“The therapeutic potential of 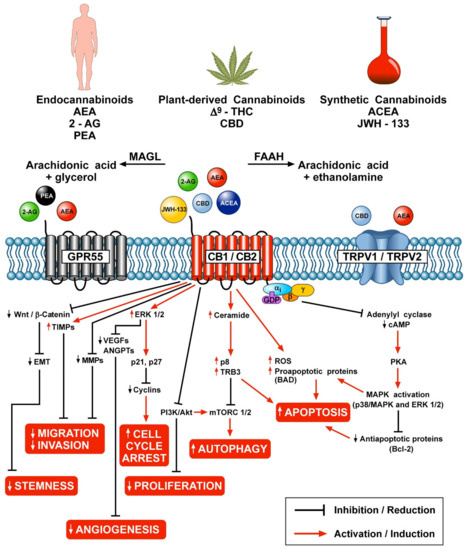
 “Cannabinoids, including delta-8- and delta-9-tetrahydrocannabinol (THC) have a palliative care impact and may therefore be beneficial against cancer.
“Cannabinoids, including delta-8- and delta-9-tetrahydrocannabinol (THC) have a palliative care impact and may therefore be beneficial against cancer.  “Background:
“Background:  “The cannabinoid, cannabidiol (CBD), is part of the plant’s natural defense system that when given to animals has many useful medicinal properties, including activity against cancer cells, modulation of the immune system, and efficacy in epilepsy.
“The cannabinoid, cannabidiol (CBD), is part of the plant’s natural defense system that when given to animals has many useful medicinal properties, including activity against cancer cells, modulation of the immune system, and efficacy in epilepsy.  “Cannabis
“Cannabis “Foodborne protein hydrolysates exhibit biological activity that may be therapeutic in a number of human disease settings. Hemp peptides (HP) generated by controlled hydrolysis of hemp proteins have a number of health benefits and are of pharmaceutical value. In the present study, we produce small molecular weight HP from hemp seed and investigate its anticancer properties in Hep3B human liver cancer cells. We demonstrate that HP treatment increased apoptosis, reduced cell viability, and reduced cell migration in Hep3B human liver cancer cells without affecting the normal liver cell line L02. We correlate these phenotypes with increased cellular ROS levels, upregulation of cleaved caspase 3 and Bad, and downregulation of antiapoptotic Bcl-2. HP treatment led to increased Akt and GSK-3β phosphorylation, with subsequent downregulation of β-catenin, suggesting β-catenin signaling modulation as a critical mechanism by which HP exhibits anticancer properties. Our findings suggest HP are of potential therapeutic interest for liver cancer treatment.”
“Foodborne protein hydrolysates exhibit biological activity that may be therapeutic in a number of human disease settings. Hemp peptides (HP) generated by controlled hydrolysis of hemp proteins have a number of health benefits and are of pharmaceutical value. In the present study, we produce small molecular weight HP from hemp seed and investigate its anticancer properties in Hep3B human liver cancer cells. We demonstrate that HP treatment increased apoptosis, reduced cell viability, and reduced cell migration in Hep3B human liver cancer cells without affecting the normal liver cell line L02. We correlate these phenotypes with increased cellular ROS levels, upregulation of cleaved caspase 3 and Bad, and downregulation of antiapoptotic Bcl-2. HP treatment led to increased Akt and GSK-3β phosphorylation, with subsequent downregulation of β-catenin, suggesting β-catenin signaling modulation as a critical mechanism by which HP exhibits anticancer properties. Our findings suggest HP are of potential therapeutic interest for liver cancer treatment.” “Cannabinoids are a family of heterogeneous compounds that mostly interact with receptors eliciting several physiological effects both in the central and peripheral nervous systems and in peripheral organs. They exert anticancer action by modulating signaling pathways involved in cancer progression; furthermore, the effects induced by their use depend on both the type of tumor and their action on the components of the endocannabinoid system. This review will explore the mechanism of action of the cannabinoids in signaling pathways involved in cancer proliferation, neovascularisation, migration, invasion, metastasis, and tumor angiogenesis.”
“Cannabinoids are a family of heterogeneous compounds that mostly interact with receptors eliciting several physiological effects both in the central and peripheral nervous systems and in peripheral organs. They exert anticancer action by modulating signaling pathways involved in cancer progression; furthermore, the effects induced by their use depend on both the type of tumor and their action on the components of the endocannabinoid system. This review will explore the mechanism of action of the cannabinoids in signaling pathways involved in cancer proliferation, neovascularisation, migration, invasion, metastasis, and tumor angiogenesis.”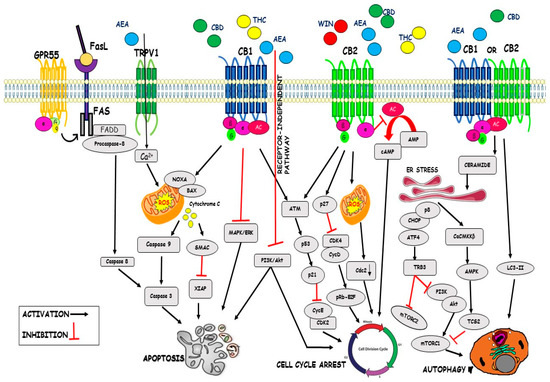
 “Agents targeting the endocannabinoid system (ECS) have gained attention as potential cancer treatments. Given recent evidence that cannabinoid receptor 2 (CB2R) regulates lymphocyte development and inflammation, we performed studies on CB2R in the immune response against melanoma. Analysis of The Cancer Genome Atlas (TCGA) data revealed a strong positive correlation between CB2R expression and survival, as well as B cell infiltration in human melanoma. In a murine melanoma model, CB2R expression reduced the growth of melanoma as well as the B cell frequencies in the tumor microenvironment (TME), compared to CB2R-deficient mice. In depth analysis of tumor-infiltrating B cells using single-cell RNA sequencing suggested a less differentiated phenotype in tumors from
“Agents targeting the endocannabinoid system (ECS) have gained attention as potential cancer treatments. Given recent evidence that cannabinoid receptor 2 (CB2R) regulates lymphocyte development and inflammation, we performed studies on CB2R in the immune response against melanoma. Analysis of The Cancer Genome Atlas (TCGA) data revealed a strong positive correlation between CB2R expression and survival, as well as B cell infiltration in human melanoma. In a murine melanoma model, CB2R expression reduced the growth of melanoma as well as the B cell frequencies in the tumor microenvironment (TME), compared to CB2R-deficient mice. In depth analysis of tumor-infiltrating B cells using single-cell RNA sequencing suggested a less differentiated phenotype in tumors from 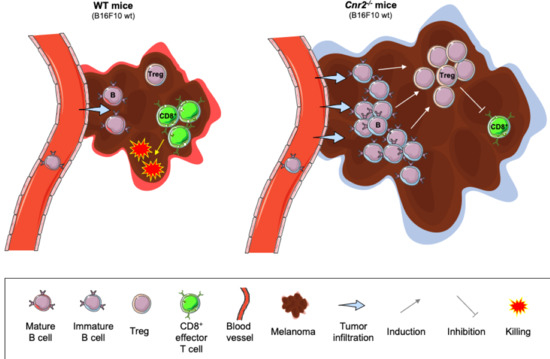
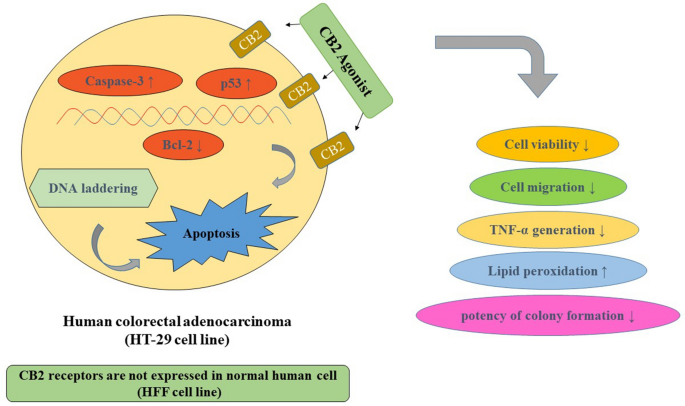
 “Colorectal cancer (CRC) is between the top three occurring cancers worldwide. The anticancer effects of Cannabinoid receptor 2 (CB
“Colorectal cancer (CRC) is between the top three occurring cancers worldwide. The anticancer effects of Cannabinoid receptor 2 (CB