“Cannabidiol (CBD) has been used to treat a variety of cancers and inflammatory conditions with controversial results. In previous work, we have shown that breast cancer MCF-7 cells, selected by their response to inflammatory IL-1β cytokine, acquire a malignant phenotype (6D cells) through an epithelial-mesenchymal transition (EMT).
“Cannabidiol (CBD) has been used to treat a variety of cancers and inflammatory conditions with controversial results. In previous work, we have shown that breast cancer MCF-7 cells, selected by their response to inflammatory IL-1β cytokine, acquire a malignant phenotype (6D cells) through an epithelial-mesenchymal transition (EMT).
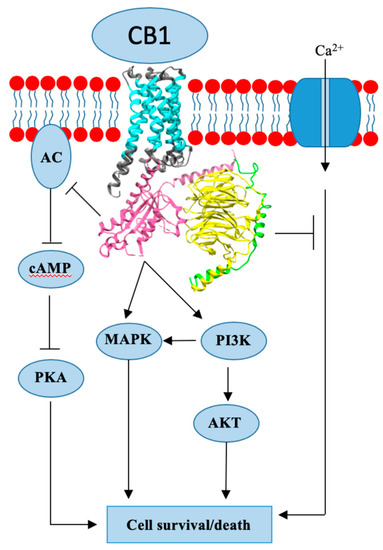
We evaluated CBD as a potential inhibitor of this transition and inducer of reversion to a non-invasive phenotype. It decreased 6D cell viability, downregulating expression of receptor CB1. The CBD blocked migration and progression of the IL-1β-induced signaling pathway IL-1β/IL-1RI/β-catenin, the driver of EMT.
Cannabidiol reestablished the epithelial organization lost by dispersion of the cells and re-localized E-cadherin and β-catenin at the adherens junctions. It also prevented β-catenin nuclear translocation and decreased over-expression of genes for ∆Np63α, BIRC3, and ID1 proteins, induced by IL-1β for acquisition of malignant features.
Cannabidiol inhibited the protein kinase B (AKT) activation, a crucial effector in the IL-1β/IL-1RI/β-catenin pathway, indicating that at this point there is crosstalk between IL-1β and CBD signaling which results in phenotype reversion.
Our 6D cell system allowed step-by-step analysis of the phenotype transition and better understanding of mechanisms by which CBD blocks and reverts the effects of inflammatory IL-1β in the EMT.”

 “The endocannabinoid system (ECS) comprises the canonical receptor subtypes CB1R and CB2R and endocannabinoids (anandamide, AEA and 2-arachidonoylglycerol, 2-AG), and a “non-canonical” extended signaling network consisting of: (i) other fatty acid derivatives; (ii) the defined “ionotropic cannabinoid receptors” (TRP channels); other GPCRs (GPR55, PPARα); (iii) enzymes involved in the biosynthesis and degradation of endocannabinoids (FAAH and MAGL); and (iv) protein transporters (FABP family).The ECS is currently a hot topic due to its involvement in cancer and pain.
“The endocannabinoid system (ECS) comprises the canonical receptor subtypes CB1R and CB2R and endocannabinoids (anandamide, AEA and 2-arachidonoylglycerol, 2-AG), and a “non-canonical” extended signaling network consisting of: (i) other fatty acid derivatives; (ii) the defined “ionotropic cannabinoid receptors” (TRP channels); other GPCRs (GPR55, PPARα); (iii) enzymes involved in the biosynthesis and degradation of endocannabinoids (FAAH and MAGL); and (iv) protein transporters (FABP family).The ECS is currently a hot topic due to its involvement in cancer and pain. “Given the infancy and evolving complexity of medicinal marijuana, an evolving political landscape, and the growing frequency of its use in cancer care, it is important for oncologists to be actively engaged in developing and successfully implementing clinical trials focusing on medical marijuana.
“Given the infancy and evolving complexity of medicinal marijuana, an evolving political landscape, and the growing frequency of its use in cancer care, it is important for oncologists to be actively engaged in developing and successfully implementing clinical trials focusing on medical marijuana. “Glioblastoma multiforme (GBM) is the most frequent and aggressive malignant brain tumour, with a poor prognosis despite available surgical and radio-chemotherapy, rising the necessity for searching alternative therapies. Several preclinical studies evaluating the efficacy of
“Glioblastoma multiforme (GBM) is the most frequent and aggressive malignant brain tumour, with a poor prognosis despite available surgical and radio-chemotherapy, rising the necessity for searching alternative therapies. Several preclinical studies evaluating the efficacy of  “The global cancer burden is significantly increasing at an alarming rate affecting patients, relatives, communities, and health-care system. Cancer patients require adequate pain relief and palliative care throughout the life course, especially in terminal illness. Although opioid treatment is successful in majority of patients, around 40% do not achieve enough analgesia or are prone to serious side effects and toxicity. The treatment of medical conditions with cannabis and
“The global cancer burden is significantly increasing at an alarming rate affecting patients, relatives, communities, and health-care system. Cancer patients require adequate pain relief and palliative care throughout the life course, especially in terminal illness. Although opioid treatment is successful in majority of patients, around 40% do not achieve enough analgesia or are prone to serious side effects and toxicity. The treatment of medical conditions with cannabis and  “The weak but noteworthy presence of (poly)phenols in hemp seeds has been long overshadowed by the essential polyunsaturated fatty acids and digestible proteins, considered responsible for their high nutritional benefits. Instead, lignanamides and their biosynthetic precursors, phenylamides, seem to display interesting and diverse biological activities only partially clarified in the last decades. Herein, negative mode HR-MS/MS techniques were applied to the chemical investigation of a (poly)phenol-rich fraction, obtained from hemp seeds after extraction/fractionation steps. This extract contained phenylpropanoid amides and their random oxidative coupling derivatives, lignanamides, which were the most abundant compounds and showed a high chemical diversity, deeply unraveled through high resolution tandem mass spectrometry (HR-MS/MS) tools.
“The weak but noteworthy presence of (poly)phenols in hemp seeds has been long overshadowed by the essential polyunsaturated fatty acids and digestible proteins, considered responsible for their high nutritional benefits. Instead, lignanamides and their biosynthetic precursors, phenylamides, seem to display interesting and diverse biological activities only partially clarified in the last decades. Herein, negative mode HR-MS/MS techniques were applied to the chemical investigation of a (poly)phenol-rich fraction, obtained from hemp seeds after extraction/fractionation steps. This extract contained phenylpropanoid amides and their random oxidative coupling derivatives, lignanamides, which were the most abundant compounds and showed a high chemical diversity, deeply unraveled through high resolution tandem mass spectrometry (HR-MS/MS) tools.
 “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).