 “Multiple therapeutic properties have been attributed to Cannabis sativa. However, further research is required to unveil the medicinal potential of Cannabis and the relationship between biological activity and chemical profile.
“Multiple therapeutic properties have been attributed to Cannabis sativa. However, further research is required to unveil the medicinal potential of Cannabis and the relationship between biological activity and chemical profile.
Objectives: The primary objective of this study was to characterize the chemical profile and antioxidant properties of three varieties of Cannabis sativa available in Uruguay during progressive stages of maturation.
Results: The main cannabinoids in the youngest inflorescences were tetrahydrocannabinolic acid (THC-A, 242 ± 62 mg/g) and tetrahydrocannabinol (THC, 7.3 ± 6.5 mg/g). Cannabinoid levels increased more than twice in two of the mature samples. A third sample showed a lower and constant concentration of THC-A and THC (177 ± 25 and 1 ± 1, respectively). The THC-A/THC rich cannabis extracts increased the latency phase of LDL oxidation by a factor of 1.2-3.5 per μg, and slowed down the propagation phase of lipoperoxidation (IC50 1.7-4.6 μg/mL). Hemp, a cannabidiol (CBD, 198 mg/g) and cannabidiolic acid (CBD-A, 92 mg/g) rich variety, also prevented the formation of conjugated dienes during LDL oxidation. In fact, 1 μg of extract was able to stretch the latency phase 3.7 times and also to significantly reduce the steepness of the propagation phase (IC50 of 8 μg/mL). Synthetic THC lengthened the duration of the lag phase by a factor of 21 per μg, while for the propagation phase showed an IC50 ≤ 1 μg/mL. Conversely, THC-A was unable to improve any parameter. Meanwhile, the presence of 1 μg of pure CBD and CBD-A increased the initial latency phase 4.8 and 9.4 times, respectively, but did not have an effect on the propagation phase.
Conclusion: Cannabis whole extracts acted on both phases of lipid oxidation in copper challenged LDL. Those effects were just partially related with the content of cannabinoids and partially recapitulated by isolated pure cannabinoids. Our results support the potentially beneficial effects of cannabis sativa whole extracts on the initial phase of atherosclerosis.”
https://pubmed.ncbi.nlm.nih.gov/33123676/
“Our findings support the beneficial effects of Cannabis sativa extracts on the initial phase of atherosclerosis. Since isolated cannabinoids were less effective preventing the oxidation of LDL, a synergistic effect between the diverse arrange of phytochemicals present in complex extracts is supported, reinforcing the entourage hypothesis and the use of whole medicinal cannabis extracts for therapeutic purposes.”
https://jcannabisresearch.biomedcentral.com/articles/10.1186/s42238-020-00042-0

 “This article provides a concise overview of how cannabinoids and the endocannabinoid system (ECS) have significant implications for the prevention and treatment of metabolic syndrome (MetS) and for the treatment of cardiovascular disorders, including cardiac fibrosis.
“This article provides a concise overview of how cannabinoids and the endocannabinoid system (ECS) have significant implications for the prevention and treatment of metabolic syndrome (MetS) and for the treatment of cardiovascular disorders, including cardiac fibrosis. “Cannabidiol (CBD) is known for its vasorelaxant (including in the human pulmonary artery), anti-proliferative and anti-inflammatory properties. The aim of our study was to examine the potential preventive effect of chronic CBD administration (10 mg/kg/day for three weeks) on monocrotaline (MCT)-induced pulmonary hypertension (PH) rats.
“Cannabidiol (CBD) is known for its vasorelaxant (including in the human pulmonary artery), anti-proliferative and anti-inflammatory properties. The aim of our study was to examine the potential preventive effect of chronic CBD administration (10 mg/kg/day for three weeks) on monocrotaline (MCT)-induced pulmonary hypertension (PH) rats.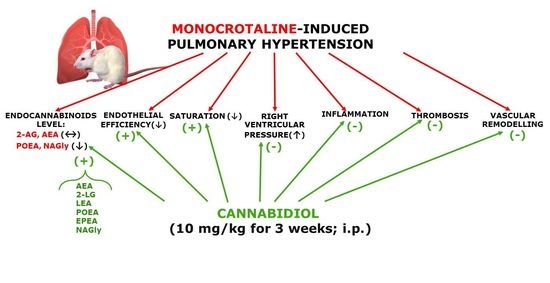
 “Chronic ethanol abuse can lead to harmful consequences for the heart, resulting in systolic dysfunction, variability in the heart rate, arrhythmia, and cardiac remodelling. However, the precise molecular mechanism responsible for ethanol-induced cardiomyopathy is poorly understood. In this regard, the present study aimed to describe the RIP1/RIP3/MLKL-mediated necroptotic cell death that may be involved in ethanol-induced cardiomyopathy and characterize CBR-mediated effects on the signalling pathway and myocardial injury.
“Chronic ethanol abuse can lead to harmful consequences for the heart, resulting in systolic dysfunction, variability in the heart rate, arrhythmia, and cardiac remodelling. However, the precise molecular mechanism responsible for ethanol-induced cardiomyopathy is poorly understood. In this regard, the present study aimed to describe the RIP1/RIP3/MLKL-mediated necroptotic cell death that may be involved in ethanol-induced cardiomyopathy and characterize CBR-mediated effects on the signalling pathway and myocardial injury. “In recent years, the role of the endocannabinoid system (ECS) in various cardiovascular conditions has been a subject of great interest. The ECS is composed of cannabinoid receptors, their endogenous ligands, also known as endocannabinoids, and enzymes responsible for the synthesis and degradation of endocannabinoids.
“In recent years, the role of the endocannabinoid system (ECS) in various cardiovascular conditions has been a subject of great interest. The ECS is composed of cannabinoid receptors, their endogenous ligands, also known as endocannabinoids, and enzymes responsible for the synthesis and degradation of endocannabinoids.
 “The study documented here was aimed to find the molecular interactions of some of the cannabinoid constituents of
“The study documented here was aimed to find the molecular interactions of some of the cannabinoid constituents of  “Increased levels of
“Increased levels of  “In vivo studies show that
“In vivo studies show that