“Background and aim: Cholangiocarcinoma (CCA) is usually diagnosed at a late stage, leading to treatment failure. Cannabidiol (CBD), exhibits diverse anti-cancer effects in various cancers, offering avenues for improving CCA treatment. This study investigated the effects of CBD on human CCA cells and the underlying mechanisms in vitro and in vivo.
Experimental procedure: The effects of CBD on three CCA cell lines (KKU-213B, KKU-100, KKU-055) were assessed using the SRB assay, clonogenic assay, cell cycle arrest, and 3D holotomography. Morphological changes were examined using transmission electron microscopy, while mitochondrial ROS levels and mitochondrial membrane potential were studied using MitoSOX, JC-1, and DCFH-DA. Cellular senescence induction was evaluated via SA-β-gal staining. Protein associatedwith autophagy and cellular senescence were analyzed using Western blot and/or immunofluorescent assays. A xenograft model demonstrated the anti-tumor activity of CBD and the induction of cellular senescence through immunohistochemistry targeting PCNA, β-gal, and p21.
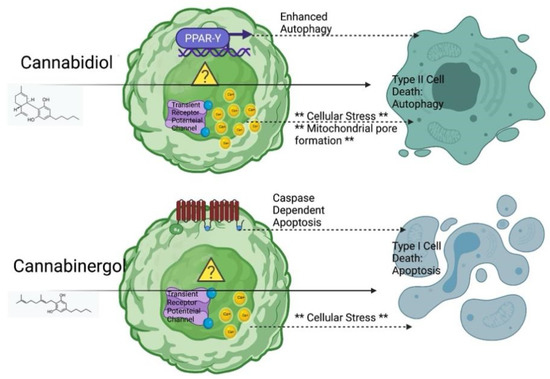
Results and conclusion: CBD effectively inhibited CCA cell proliferation, suppressed colony formation and induced G0/G1 phase cell cycle arrest. Morphological examination revealed lipid droplets/vesicles in CCA cell lines. CBD induced autophagy by upregulating LC3BII, downregulating p62, and inhibiting the p-PI3K, p-AKT, and p-mTOR pathways. Additionally, CBD disrupted mitochondrial homeostasis by elevating ROS, reducing membrane potential, and induced cellular senescence by increasing the expression of p53 and p21. In-vitro results were confirmed by xenograft models. Overall, CBD suppresses proliferation and induces cell death, autophagy and senescence in CCA cells via the PI3K/AKT/mTOR pathway, which indicates a therapeutic option for CCA treatment.”
https://pubmed.ncbi.nlm.nih.gov/39850601/
“Although CBD has shown anti-tumor activity in various solid tumors, including CCA, its mechanism of action remains poorly understood.”
“The study reported here has shown that CBD has a significant anti-tumor effect on CCA cells through various mechanisms, including the inhibition of cell proliferation both in vitro and in vivo, the reduction of colony formation ability and the induction of multiple cellular processes, notably autophagy, cell cycle arrest, cellular senescence, mitochondrial dysfunction, lipid droplet formation, and ROS overproduction.
The significant findings from our study strongly suggest that CBD, through its targeting of the PI3K/AKT/mTOR pathway, holds great promise as a therapeutic agent for treating CCA and potentially other cancers.”
“Various herbal agents, including CBD, have shown promise for the treatment of CCA.”
https://www.sciencedirect.com/science/article/pii/S2225411024000506?via%3Dihub