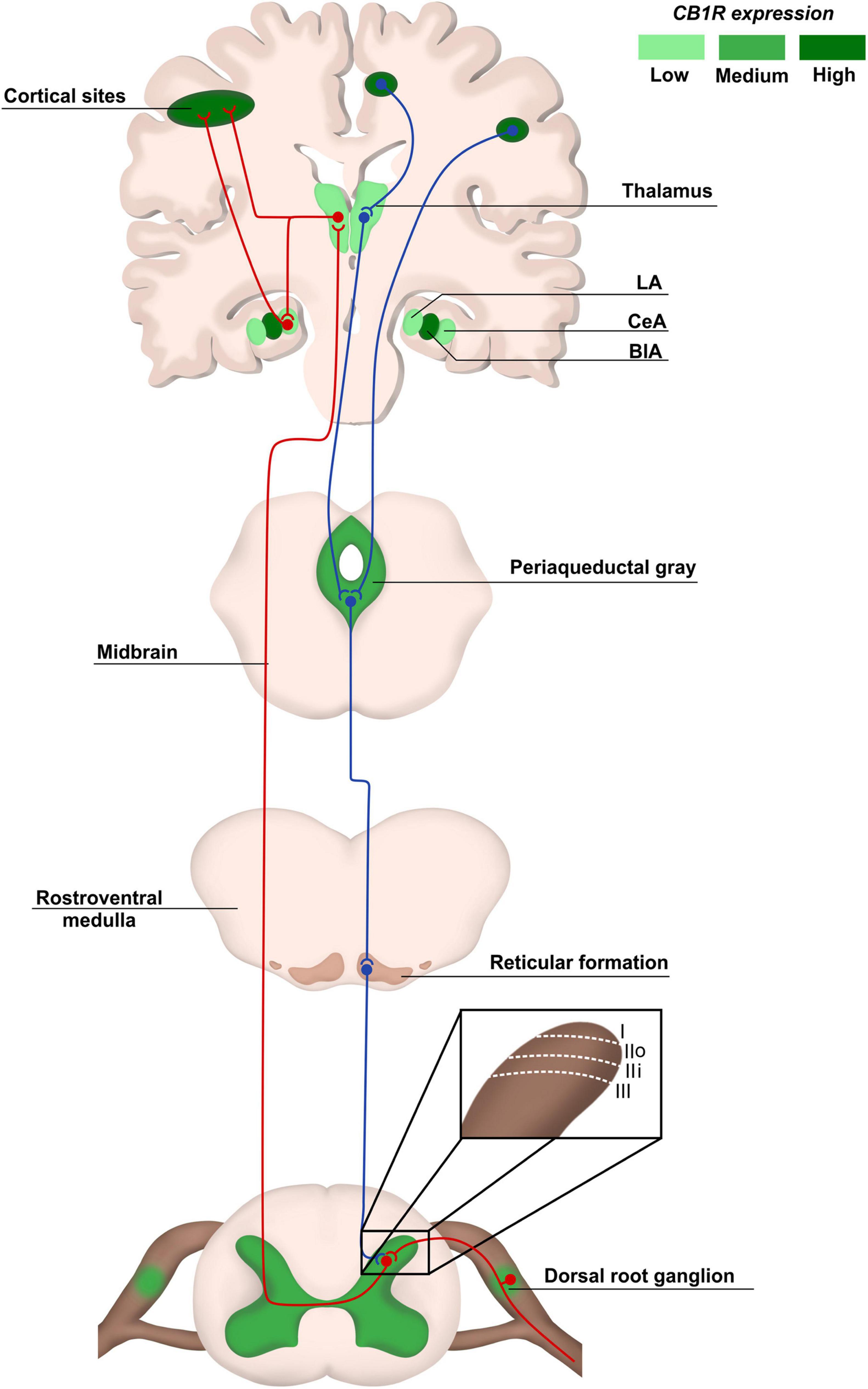
“Combination tetrahydrocannabinol (THC)/cannabidiol (CBD) medicines or CBD-only medicines are prospective treatments for chronic pain, stress, anxiety, depression, and insomnia. THC and CBD increase signaling from cannabinoid receptors, which reduces synaptic transmission in parts of the central and peripheral nervous systems and reduces the secretion of inflammatory factors from immune and glial cells.
The overall effect of adding CBD to THC medicines is to enhance the analgesic effect but counteract some of the adverse effects. There is substantial evidence for the effectiveness of THC/CBD combination medicines for chronic pain, especially neuropathic and nociplastic pain or pain with an inflammatory component. For CBD-only medication, there is substantial evidence for stress, moderate evidence for anxiety and insomnia, and minimal evidence for depression and pain.
THC/CBD combination medicines have a good tolerability and safety profile relative to opioid analgesics and have negligible dependence and abuse potential; however, should be avoided in patients predisposed to depression, psychosis and suicide as these conditions appear to be exacerbated. Non-serious adverse events are usually dose-proportional, subject to tachyphylaxis and are rarely dose limiting when patients are commenced on a low dose with gradual up-titration. THC and CBD inhibit several Phase I and II metabolism enzymes, which increases the exposure to a wide range of drugs and appropriate care needs to be taken. Low-dose CBD that appears effective for chronic pain and mental health has good tolerability and safety, with few adverse effects and is appropriate as an initial treatment.”
https://pubmed.ncbi.nlm.nih.gov/35796920/
“Tetrahydrocannabinol (THC) and cannabidiol (CBD) combination medicines and CBD-only medicines are prospective new treatments for chronic pain, stress, anxiety, depression, and insomnia, which are all medical conditions in need of better therapeutics. Both THC/CBD combination and CBD-only medicines could provide effective new treatment options for pain and mental health, respectively, and both have good safety and tolerability profiles relative to the current treatments.
THC and CBD combination medicines have a good safety and tolerability profile that is appropriate for opioid stage (stage 2–3) treatment of chronic pain. Low-dose CBD could be used as an initial treatment for chronic pain and for stress, anxiety, depression, and insomnia. High quality efficacy evidence is best for THC/CBD combination medicines for chronic pain and CBD-only medicines for stress and anxiety. “
https://link.springer.com/article/10.1007/s10787-022-01020-z