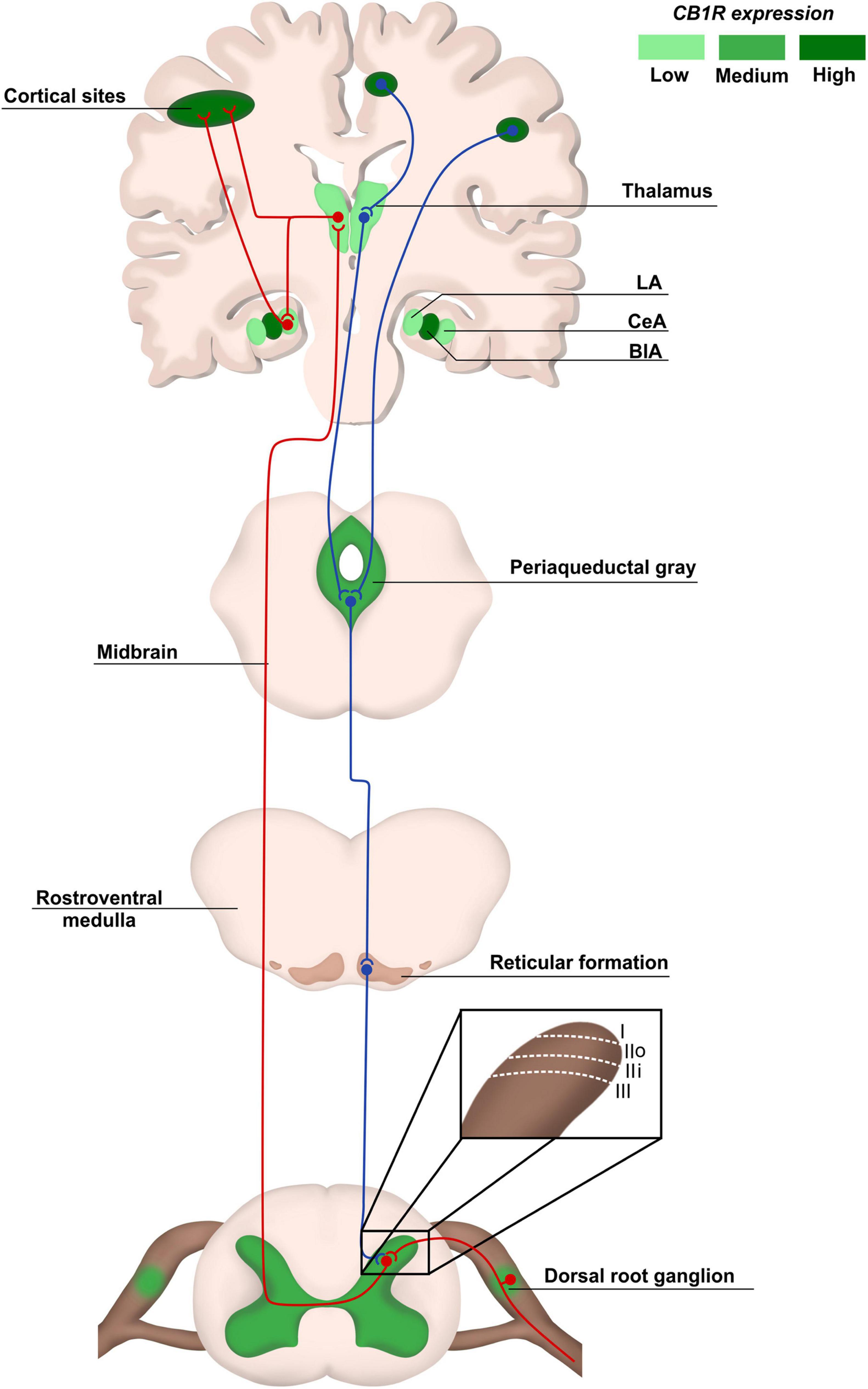
“The development of a high-end cannabinoid-based therapy is the result of intense translational research, aiming to convert recent discoveries in the laboratory into better treatments for patients. Novel compounds and new regimes for drug treatment are emerging. Given that previously unreported signaling mechanisms for cannabinoids have been uncovered, clinical studies detailing their high therapeutic potential are mandatory. The advent of novel genomic, optogenetic, and viral tracing and imaging techniques will help to further detail therapeutically relevant functional and structural features. An evolutionarily highly conserved group of neuromodulatory lipids, their receptors, and anabolic and catabolic enzymes are involved in a remarkable variety of physiological and pathological processes and has been termed the endocannabinoid system (ECS). A large body of data has emerged in recent years, pointing to a crucial role of this system in the regulation of the behavioral domains of acquired fear, anxiety, and stress-coping. Besides neurons, also glia cells and components of the immune system can differentially fine-tune patterns of neuronal activity. Dysregulation of ECS signaling can lead to a lowering of stress resilience and increased incidence of psychiatric disorders. Chronic pain may be understood as a disease process evoked by fear-conditioned nociceptive input and appears as the dark side of neuronal plasticity. By taking a toll on every part of your life, this abnormal persistent memory of an aversive state can be more damaging than its initial experience. All strategies for the treatment of chronic pain conditions must consider stress-related comorbid conditions since cognitive factors such as beliefs, expectations, and prior experience (memory of pain) are key modulators of the perception of pain. The anxiolytic and anti-stress effects of medical cannabinoids can substantially modulate the efficacy and tolerability of therapeutic interventions and will help to pave the way to a successful multimodal therapy. Why some individuals are more susceptible to the effects of stress remains to be uncovered. The development of personalized prevention or treatment strategies for anxiety and depression related to chronic pain must also consider gender differences. An emotional basis of chronic pain opens a new horizon of opportunities for developing treatment strategies beyond the repeated sole use of acutely acting analgesics. A phase I trial to determine the pharmacokinetics, psychotropic effects, and safety profile of a novel nanoparticle-based cannabinoid spray for oromucosal delivery highlights a remarkable innovation in galenic technology and urges clinical studies further detailing the huge therapeutic potential of medical cannabis (Lorenzl et al.; this issue).”
https://pubmed.ncbi.nlm.nih.gov/35702403/
“The evidence that full-spectrum cannabis preparations have medical benefits with less unwanted central effects stimulated the development of an oromucosal spray containing full-spectrum water-soluble cannabis. This remarkable innovation in galenic technology advocates clinical studies further and enables the realization of the very promising therapeutic potentials. Medicinal cannabis has a favorable safety and tolerability profile”