




 “Cannabis has been used for its medicinal purposes since ancient times. Its consumption leads to the activation of Cannabis receptors CB1 and CB2 that, through specific mechanisms can lead to modulation and progression of inflammation or repair. The novel findings are linked to the medical use of Cannabis in gastrointestinal (GI) system.
“Cannabis has been used for its medicinal purposes since ancient times. Its consumption leads to the activation of Cannabis receptors CB1 and CB2 that, through specific mechanisms can lead to modulation and progression of inflammation or repair. The novel findings are linked to the medical use of Cannabis in gastrointestinal (GI) system.
Purpose: The objective of the present paper is to elucidate the role of Cannabis consumption in GI system. An additional aim is to review the information on the function of Cannabis in non-alcoholic fatty liver disease (NAFLD).
Methods and results: This review summarizes the recent findings on the role of cannabinoid receptors, their synthetic or natural ligands, as well as their metabolizing enzymes in normal GI function and its disorders, including irritable bowel syndrome (IBS), inflammatory bowel disease (IBD) and possible adverse events. The synergism or antagonism between Cannabis’ active ingredients and the “entourage” plays a role in the efficacy of various strains. Some elements of Cannabis may alter disease severity as over-activation of Cannabis receptors CB1 and CB2 can lead to changes of the commensal gut flora. The endocannabinoid system (ECS) contributes to gut homeostasis. The ability of ECS to modulate inflammatory responses demonstrates the capacity of ECS to preserve gastrointestinal (GI) function. Alterations of the ECS may predispose patients to pathologic disorders, including IBD. Clinical studies in IBD demonstrate that subjects benefit from Cannabis consumption as seen through a reduction of the IBD-inflammation, as well as through a decreased need for other medication. NAFLD is characterized by fat accumulation in the liver. The occurrence of inflammation in NAFLD leads to non-alcoholic-steatohepatitis (NASH). The use of Cannabis might reduce liver inflammation.
Conclusions: With limited evidence of efficacy and safety of Cannabis in IBD, IBS, and NAFLD, randomized controlled studies are required to examine its therapeutic efficacy.”
https://pubmed.ncbi.nlm.nih.gov/32762830/
https://journals.library.ualberta.ca/jpps/index.php/JPPS/article/view/31242
 “The cannabis plant has been widely researched for many therapeutic indications and found to be effective in many chronic conditions such as epilepsy, neuropathic or chronic pain and more. However, biased opinion against compounds of the plant, regulatory as well as compounding challenges have led to very few approved medicinal products. Those formulations which are approved are dosed several times a day, creating an unmet need for controlled release (CR) formulations of cannabinoids. Conventional CR formulations rely on prolonged absorption including the colon. The purpose of this work is to investigate regional absorption of major cannabinoids THC and CBD from the colon and develop a suitable CR formulation. As hypothesized by researchers, THC and CBD have poor absorption from the colon compared to small intestine, suggesting that these compounds have a narrow absorption window. The suggested formulation examined in-vitro was a floating gastro retentive tablet based on egg albumin matrix, gas generating agents and surfactants. In-vivo investigation of CBD containing formulation in the freely moving rat model proved a prolonged absorption phase with a substantial increase in bioavailability compared to CBD solution. The findings of this paper answer a crucial question regarding potential application of CR dosage forms for cannabinoids and shed light on the regional intestinal absorption of these compounds. Ultimately, these results cement the way for future development of cannabinoid gastro retentive dosage forms.”
“The cannabis plant has been widely researched for many therapeutic indications and found to be effective in many chronic conditions such as epilepsy, neuropathic or chronic pain and more. However, biased opinion against compounds of the plant, regulatory as well as compounding challenges have led to very few approved medicinal products. Those formulations which are approved are dosed several times a day, creating an unmet need for controlled release (CR) formulations of cannabinoids. Conventional CR formulations rely on prolonged absorption including the colon. The purpose of this work is to investigate regional absorption of major cannabinoids THC and CBD from the colon and develop a suitable CR formulation. As hypothesized by researchers, THC and CBD have poor absorption from the colon compared to small intestine, suggesting that these compounds have a narrow absorption window. The suggested formulation examined in-vitro was a floating gastro retentive tablet based on egg albumin matrix, gas generating agents and surfactants. In-vivo investigation of CBD containing formulation in the freely moving rat model proved a prolonged absorption phase with a substantial increase in bioavailability compared to CBD solution. The findings of this paper answer a crucial question regarding potential application of CR dosage forms for cannabinoids and shed light on the regional intestinal absorption of these compounds. Ultimately, these results cement the way for future development of cannabinoid gastro retentive dosage forms.”
https://www.ncbi.nlm.nih.gov/pubmed/32422168
https://www.sciencedirect.com/science/article/abs/pii/S0939641120301375?via%3Dihub
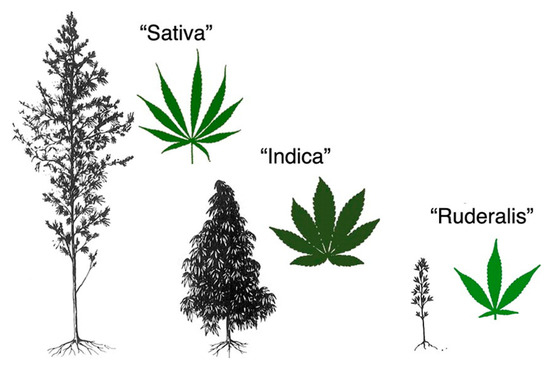
 “Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
“Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
Phytocannabinoids (terpenophenolic compounds derived from the plant), include the well-known psychoactive cannabinoid Δ9-tetrahydrocannabinol, and many non-psychoactive cannabinoids, like cannabidiol.
The endocannabinoid system (ECS) comprises of endocannabinoid ligands, enzymes for synthesis and degradation of such ligands, and receptors. This system is widely distributed in the gastrointestinal tract, where phytocannabinoids exert potent effects, particularly under pathological (i.e., inflammatory) conditions.
Herein, we will first look at the hemp plant as a possible source of new functional food ingredients and nutraceuticals that might be eventually useful to treat or even prevent gastrointestinal conditions.
Subsequently, we will briefly describe the ECS and the general pharmacology of phytocannabinoids. Finally, we will revise the available data showing that non-psychoactive phytocannabinoids, particularly cannabidiol, may be useful to treat different disorders and diseases of the gastrointestinal tract.
With the increasing interest in the development of functional foods for a healthy life, the non-psychoactive phytocannabinoids are hoped to find a place as nutraceuticals and food ingredients also for a healthy gastrointestinal tract function.”
https://www.ncbi.nlm.nih.gov/pubmed/32357565
https://www.mdpi.com/1422-0067/21/9/3067
 “Many anti-nausea treatments are available for chronic gastrointestinal syndromes, but data on efficacy and comparative effectiveness are sparse.
“Many anti-nausea treatments are available for chronic gastrointestinal syndromes, but data on efficacy and comparative effectiveness are sparse.
To conduct a sectional survey study of patients with chronic nausea to assess comparative effectiveness of commonly used anti-nausea treatments.
One hundred and fifty-three patients completed the survey. The mean efficacy score of all anti-nausea treatments evaluated was 1.73. After adjustment, three treatments had scores statically higher than the mean, including marijuana (2.75, p < 0.0001), ondansetron (2.64, p < 0.0001), and promethazine (2.46, p < 0.0001). Several treatments, including many neuromodulators, complementary and alternative treatments, erythromycin, and diphenhydramine had scores statistically below average. Patients with more severe nausea responded better to marijuana (p = 0.036) and diphenhydramine (p < 0.001) and less so to metoclopramide (p = 0.020). There was otherwise no significant differential response by age, gender, nausea localization, underlying gastrointestinal cause of nausea, and GCSI.
When treating nausea in patients with chronic gastrointestinal syndromes, clinicians may consider trying higher performing treatments first, and forgoing lower performing treatments. Further prospective research is needed, particularly with respect to highly effective treatments.”
https://www.ncbi.nlm.nih.gov/pubmed/32185665
https://link.springer.com/article/10.1007%2Fs10620-020-06195-5
 “Chronic intestinal pseudo-obstruction (CIPO) is a rare and challenging cause of pediatric intestinal failure, requiring long-term parenteral nutrition in most cases. Despite optimal management, some patients experience chronic abdominal pain and recurrent obstructive episodes with a major impact on their quality of life.
“Chronic intestinal pseudo-obstruction (CIPO) is a rare and challenging cause of pediatric intestinal failure, requiring long-term parenteral nutrition in most cases. Despite optimal management, some patients experience chronic abdominal pain and recurrent obstructive episodes with a major impact on their quality of life.
Cannabinoids have been successfully used in some conditions. However, their use in CIPO has never been reported in the literature.
We report a case of successful use of medicinal cannabinoids in a patient with CIPO, resulting in a significant reduction of abdominal pain, vomiting, and subocclusive episodes and increased appetite and weight, without major adverse events.
Although further observations are required to consolidate these findings, this case may be helpful for other patients suffering from the same condition.”
 “A growing body of literature indicates that activation of cannabinoid receptors may exert beneficial effects on gastrointestinal inflammation and visceral hypersensitivity.
“A growing body of literature indicates that activation of cannabinoid receptors may exert beneficial effects on gastrointestinal inflammation and visceral hypersensitivity.
The present study aimed to immunohistochemically investigate the distribution of the canonical cannabinoid receptors CB1 (CB1R) and CB2 (CB2R) and the putative cannabinoid receptors G protein-coupled receptor 55 (GPR55), nuclear peroxisome proliferator-activated receptor alpha (PPARα), transient receptor potential ankyrin 1 (TRPA1), and serotonin receptor 5-HT1a 5-HT1aR) in tissue samples of the gastrointestinal tract of the cat.
CB1R-immunoreactivity (CB1R-IR) was observed in gastric epithelial cells, intestinal enteroendocrine cells (EECs) and goblet cells, lamina propria mast cells (MCs), and enteric neurons. CB2R-IR was expressed by EECs, enterocytes, and macrophages. GPR55-IR was expressed by EECs, macrophages, immunocytes, and MP neurons. PPARα-IR was expressed by immunocytes, smooth muscle cells, and enteroglial cells. TRPA1-IR was expressed by enteric neurons and intestinal goblet cells. 5-HT1a receptor-IR was expressed by gastrointestinal epithelial cells and gastric smooth muscle cells.
Cannabinoid receptors showed a wide distribution in the feline gastrointestinal tract layers. Although not yet confirmed/supported by functional evidences, the present research might represent an anatomical substrate potentially useful to support, in feline species, the therapeutic use of cannabinoids during gastrointestinal inflammatory diseases.”
“Cannabinoids are increasingly used for medicinal purposes, including neuropathy.
Gastroparesis is a neuromuscular disorder and neuropathy plays a large role in its pathogenesis. It is thus reasonable that cannabinoids can serve a beneficial role in the management of gastroparesis.
Our study evaluates the effect of cannabinoids on gastroparesis symptoms.
A significant improvement in the GCSI total symptom composite score was seen with either cannabinoid treatment (mean score difference of 12.8, 95% confidence interval 10.4-15.2; p-value < 0. 001). Patients prescribed marijuana experienced a statistically significant improvement in every GCSI symptom subgroup. Significant improvement in abdominal pain score was also seen with either cannabinoid treatment (mean score difference of 1.6; p-value <0.001).
Conclusions: Cannabinoids dramatically improve the symptoms of gastroparesis. Furthermore, an improvement in abdominal pain with cannabinoids represents a breakthrough for gastroparesis-associated abdominal pain treatment, for which there are currently no validated therapies.”
https://www.ncbi.nlm.nih.gov/pubmed/31993268
“In conclusion, cannabinoids dramatically improve refractory gastroparesis symptoms, including abdominal pain. Marijuana may be superior to dronabinol in improving these symptoms, though both cannabinoids seem to be promising as novel therapeutic options in gastroparesis.”
 “Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies.
“Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies.
The Endocannabinoid system (ECS) of our body plays a key role in maintaining normal physiology of the gastrointestinal tract as well as involves abnormalities including functional diseases like IBS. This review highlights the importance of the Endocannabinoid system, its connections with the normal gastrointestinal functions and abnormalities like IBS.
It also discusses the role of cannabis as medical therapy in IBS patients.
A literature search for articles related to endocannabinoids in IBS and medical cannabis in PubMed and Google Scholar was conducted. The studies highlighted the significant participation of ECS in IBS. However, the breach in obtaining the promising therapeutic model for IBS needed further investigation in ECS and uncover other treatments for IBS.
This review summarizes ECS, highlights the relationship of ECS with IBS and explores cannabis as a potential therapy to treat IBS.”
https://www.ncbi.nlm.nih.gov/pubmed/31987224
https://www.sciencedirect.com/science/article/pii/S0965229919310179?via%3Dihub
 “Irritable bowel syndrome (IBS) is one of the most common functional gastrointestinal (GI) disorders characterized by pain and impaired bowel movements. Currently available drugs show limited efficacy.
“Irritable bowel syndrome (IBS) is one of the most common functional gastrointestinal (GI) disorders characterized by pain and impaired bowel movements. Currently available drugs show limited efficacy.
Cannabinoid 1 receptor (CB1) inverse agonists (CB1-RAN) cause diarrhea and may be candidates for the treatment of constipation-predominant IBS (IBS-C). We evaluated the effects of CB1-RAN in clinical trials for their potential use in IBS-C.
Database search identified all clinical trials published up to May 2018 that reported rimonabant and taranabant treatment for at least one month and detailed the GI adverse events (AEs). Categorical outcomes (subgroups of AEs) were analyzed using the odds ratio (OR).
Eighteen trials met the inclusion criteria. Rimonabant 20 mg produced significantly more overall AEs (OR=1.35, CI: 1.19-1.52, p<0.0001), psychiatric events (OR=1.79, CI: 1.46-2.21, p<0.001) and GI AEs (OR=2.05, CI: 1.65-2.55, p<0.001) compared to placebo. Taranabant at doses ranging from 0.5 to 8 mg produced significantly more overall AEs (OR=1.36, CI: 1.13-1.64, p<0.002), psychiatric AEs (1.82, CI: 1.54-2.16, p<0.001) and GI AEs (OR=1.75, CI: 1.29-2.37, p<0.001) compared to placebo.
The approach to target CB1 in the gut for the treatment of IBS-C or chronic constipation seems a promising therapeutic option. Prospective clinical trials on the possible targeting of CB1 and the endocannabinoid system are warranted.”