“The potential medicinal properties of Cannabis continue to garner attention, especially in the brain tumor domain. This attention is centered on quality of life and symptom management; however, it is amplified by a significant lack of therapeutic choices for this specific patient population.
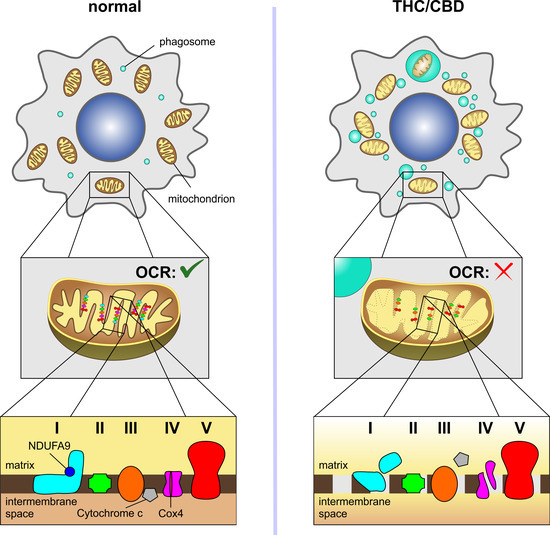
While the literature on this matter is young, published and anecdotal evidence imply that cannabis could be useful in treating chemotherapy-induced nausea and vomiting, stimulating appetite, reducing pain, and managing seizures. It may also decrease inflammation and cancer cell proliferation and survival, resulting in a benefit in overall patient survival.
Current literature poses the challenge that it does not provide standardized guidance on dosing for the above potential indications and cannabis use is dominated by recreational purposes. Furthermore, integrated and longitudinal studies are needed but these are a challenge due to arcane laws surrounding the legality of such substances. The increasing need for evidence-based arguments about potential harms and benefits of cannabis, not only in cancer patients but for other medical use and recreational purposes, is desperately needed.”
https://pubmed.ncbi.nlm.nih.gov/36633803/
https://link.springer.com/article/10.1007/s11864-022-01047-y