 “People living with HIV (PLWH) report higher rates of cannabis use than the general population, a trend likely to continue in light of recent policy changes and the reported therapeutic benefits of cannabis for PLWH. Therefore, it is important to better understand cannabis-associated effects on neurocognition, especially as PLWH are at heightened risk for neurocognitive impairment.
“People living with HIV (PLWH) report higher rates of cannabis use than the general population, a trend likely to continue in light of recent policy changes and the reported therapeutic benefits of cannabis for PLWH. Therefore, it is important to better understand cannabis-associated effects on neurocognition, especially as PLWH are at heightened risk for neurocognitive impairment.
This study aimed to elucidate the effects of a past cannabis use disorder on current neurocognition in a diverse sample of PLWH.
Compared to the past CUD- group, the past CUD+ group performed significantly better on tests of processing speed, visual learning and memory, and motor ability.
Findings suggest PLWH with past cannabis use have similar or better neurocognition across domains compared to PLWH without past use.”
https://pubmed.ncbi.nlm.nih.gov/32951441/
https://www.tandfonline.com/doi/abs/10.1080/09540121.2020.1822504?journalCode=caic20

 “Current literature on the effect of cannabis use on sleep quality is mixed, and few studies have used objectively-measured sleep measures or real-time sampling of cannabis use to examine this relationship.
“Current literature on the effect of cannabis use on sleep quality is mixed, and few studies have used objectively-measured sleep measures or real-time sampling of cannabis use to examine this relationship. “HIV is associated with disruptions in cognition and brain function.
“HIV is associated with disruptions in cognition and brain function. “HIV/SIV-associated oral mucosal disease/dysfunction (HAOMD) (gingivitis/periodontitis/salivary adenitis) represents a major comorbidity affecting HIV patients on anti-retroviral therapy.
“HIV/SIV-associated oral mucosal disease/dysfunction (HAOMD) (gingivitis/periodontitis/salivary adenitis) represents a major comorbidity affecting HIV patients on anti-retroviral therapy. “Objective: To determine whether cannabis may reduce HIV-related persistent inflammation, we evaluated the relationship of cannabis use in people with HIV (PWH) to inflammatory cytokines in CSF and blood plasma.
“Objective: To determine whether cannabis may reduce HIV-related persistent inflammation, we evaluated the relationship of cannabis use in people with HIV (PWH) to inflammatory cytokines in CSF and blood plasma. “HIV infection affects an estimated 38 million people. Approximately 50% of HIV patients exhibit neurocognitive dysfunction termed HIV-Associated Neurocognitive Disorder (HAND). HAND is a consequence of chronic low-level neuroinflammation due to HIV entry into the brain. Initially, monocytes become activated in circulation and traffic to the brain. Monocytes, when activated, become susceptible to infection by HIV and can then carry the virus across the blood brain barrier. Once in the brain, activated monocytes secrete chemokines, which recruit virus-specific CD8+ T cells into the brain to further promote neuroinflammation. HAND is closely linked to systemic inflammation driven, in part, by HIV but is also due to persistent translocation of microorganisms across the GI tract. Persistent anti-viral responses in the GI tract compromise microbial barrier integrity. Indeed, HIV patients can exhibit remarkably high levels of activated (CD16+) monocytes in circulation.
“HIV infection affects an estimated 38 million people. Approximately 50% of HIV patients exhibit neurocognitive dysfunction termed HIV-Associated Neurocognitive Disorder (HAND). HAND is a consequence of chronic low-level neuroinflammation due to HIV entry into the brain. Initially, monocytes become activated in circulation and traffic to the brain. Monocytes, when activated, become susceptible to infection by HIV and can then carry the virus across the blood brain barrier. Once in the brain, activated monocytes secrete chemokines, which recruit virus-specific CD8+ T cells into the brain to further promote neuroinflammation. HAND is closely linked to systemic inflammation driven, in part, by HIV but is also due to persistent translocation of microorganisms across the GI tract. Persistent anti-viral responses in the GI tract compromise microbial barrier integrity. Indeed, HIV patients can exhibit remarkably high levels of activated (CD16+) monocytes in circulation.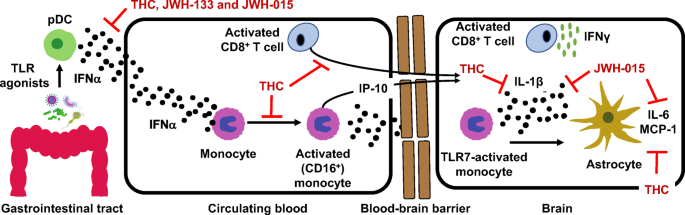
 “HIV infection leads to blood-brain barrier (BBB) dysfunction that does not resolve despite viral suppression on antiretroviral therapy and is associated with adverse clinical outcomes.
“HIV infection leads to blood-brain barrier (BBB) dysfunction that does not resolve despite viral suppression on antiretroviral therapy and is associated with adverse clinical outcomes. “Neuropathic pain associated with nucleoside reverse transcriptase inhibitors (NRTIs), therapeutic agents for human immunodeficiency virus (HIV), responds poorly to available drugs.
“Neuropathic pain associated with nucleoside reverse transcriptase inhibitors (NRTIs), therapeutic agents for human immunodeficiency virus (HIV), responds poorly to available drugs. “Aging and HIV have adverse effects on the central nervous system, including increased inflammation and neural injury and confer risk of neurocognitive impairment (NCI).
“Aging and HIV have adverse effects on the central nervous system, including increased inflammation and neural injury and confer risk of neurocognitive impairment (NCI). “HIV-associated neurocognitive disorder (HAND) affects nearly half of all HIV-infected individuals. Synaptodendritic damage correlates with neurocognitive decline in HAND, and many studies have demonstrated that HIV-induced neuronal injury results from excitotoxic and inflammatory mechanisms.
“HIV-associated neurocognitive disorder (HAND) affects nearly half of all HIV-infected individuals. Synaptodendritic damage correlates with neurocognitive decline in HAND, and many studies have demonstrated that HIV-induced neuronal injury results from excitotoxic and inflammatory mechanisms.