“Cannabis sativa L. turned out to be a valuable source of chemical compounds of various structures, showing pharmacological activity. The most important groups of compounds include phytocannabinoids and terpenes.
“Cannabis sativa L. turned out to be a valuable source of chemical compounds of various structures, showing pharmacological activity. The most important groups of compounds include phytocannabinoids and terpenes.
The pharmacological activity of Cannabis (in epilepsy, sclerosis multiplex (SM), vomiting and nausea, pain, appetite loss, inflammatory bowel diseases (IBDs), Parkinson’s disease, Tourette’s syndrome, schizophrenia, glaucoma, and coronavirus disease 2019 (COVID-19)), which has been proven so far, results from the affinity of these compounds predominantly for the receptors of the endocannabinoid system (the cannabinoid receptor type 1 (CB1), type two (CB2), and the G protein-coupled receptor 55 (GPR55)) but, also, for peroxisome proliferator-activated receptor (PPAR), glycine receptors, serotonin receptors (5-HT), transient receptor potential channels (TRP), and GPR, opioid receptors.
The synergism of action of phytochemicals present in Cannabis sp. raw material is also expressed in their increased bioavailability and penetration through the blood-brain barrier. This review provides an overview of phytochemistry and pharmacology of compounds present in Cannabis extracts in the context of the current knowledge about their synergistic actions and the implications of clinical use in the treatment of selected diseases.”
https://www.mdpi.com/1422-0067/22/2/778

 “The relevance and incidence of intestinal bowel diseases (IBD) have been increasing over the last 50 years and the current therapies are characterized by severe side effects, making essential the development of new strategies that combine efficacy and safety in the management of human IBD. Herbal products are highly considered in research aimed at discovering new approaches for IBD therapy and, among others,
“The relevance and incidence of intestinal bowel diseases (IBD) have been increasing over the last 50 years and the current therapies are characterized by severe side effects, making essential the development of new strategies that combine efficacy and safety in the management of human IBD. Herbal products are highly considered in research aimed at discovering new approaches for IBD therapy and, among others, 

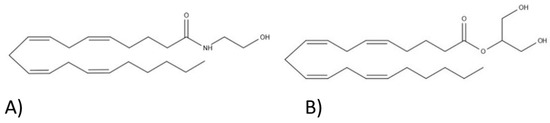
 “Fish oil (FO) and phytocannabinoids have received considerable attention for their intestinal anti-inflammatory effects.
“Fish oil (FO) and phytocannabinoids have received considerable attention for their intestinal anti-inflammatory effects. “Cannabis has been used for its medicinal purposes since ancient times. Its consumption leads to the activation of Cannabis receptors CB1 and CB2 that, through specific mechanisms can lead to modulation and progression of inflammation or repair. The novel findings are linked to the medical use of Cannabis in gastrointestinal (GI) system.
“Cannabis has been used for its medicinal purposes since ancient times. Its consumption leads to the activation of Cannabis receptors CB1 and CB2 that, through specific mechanisms can lead to modulation and progression of inflammation or repair. The novel findings are linked to the medical use of Cannabis in gastrointestinal (GI) system. “Irritable bowel syndrome (IBS) is a frequent cause of abdominal pain and altered bowel habits, which is associated with significant healthcare utilization.
“Irritable bowel syndrome (IBS) is a frequent cause of abdominal pain and altered bowel habits, which is associated with significant healthcare utilization. “Inflammatory Bowel Disease (IBD) is idiopathic, chronic and affects the gastrointestinal tract. It results from the association of genetic, environmental and immune deregulation, which culminates in the development and progression of the inflammatory process. In an attempt to reverse colonic inflammation, endogenous systems involved in intestinal physiology are studied and the cholinergic system is fundamental for this process. In addition, this system has anti-inflammatory action in experimental models of IBD. Another important endogenous system in regulating the exacerbated inflammatory response in the gut is mediated by endocannabinoids, which play an important role in restoring bowel functionality after the onset of the inflammatory process. There are several reports in the literature showing the interconnection between the cannabinoid and cholinergic systems in different tissues. Considering that the activation of the cholinergic system stimulates the production of cannabinoid agonists in the intestine, our hypothesis is that the interaction between the muscarinic system and the cannabinoid in the control of intestinal inflammation is mediated by endogenous cannabinoids, since they are stimulated by the activation of muscarinic receptors.”
“Inflammatory Bowel Disease (IBD) is idiopathic, chronic and affects the gastrointestinal tract. It results from the association of genetic, environmental and immune deregulation, which culminates in the development and progression of the inflammatory process. In an attempt to reverse colonic inflammation, endogenous systems involved in intestinal physiology are studied and the cholinergic system is fundamental for this process. In addition, this system has anti-inflammatory action in experimental models of IBD. Another important endogenous system in regulating the exacerbated inflammatory response in the gut is mediated by endocannabinoids, which play an important role in restoring bowel functionality after the onset of the inflammatory process. There are several reports in the literature showing the interconnection between the cannabinoid and cholinergic systems in different tissues. Considering that the activation of the cholinergic system stimulates the production of cannabinoid agonists in the intestine, our hypothesis is that the interaction between the muscarinic system and the cannabinoid in the control of intestinal inflammation is mediated by endogenous cannabinoids, since they are stimulated by the activation of muscarinic receptors.” “Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies.
“Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies. “Irritable bowel syndrome (IBS) is one of the most common functional gastrointestinal (GI) disorders characterized by pain and impaired bowel movements. Currently available drugs show limited efficacy.
“Irritable bowel syndrome (IBS) is one of the most common functional gastrointestinal (GI) disorders characterized by pain and impaired bowel movements. Currently available drugs show limited efficacy.