 “Cannabidiol (CBD) is a non-psychoactive phytocannabinoid known for its beneficial effects including antioxidant and anti-inflammatory properties. Moreover, CBD is a compound with antidepressant, anxiolytic, anticonvulsant and antipsychotic effects. Thanks to all these properties, the interest of the scientific community for it has grown.
“Cannabidiol (CBD) is a non-psychoactive phytocannabinoid known for its beneficial effects including antioxidant and anti-inflammatory properties. Moreover, CBD is a compound with antidepressant, anxiolytic, anticonvulsant and antipsychotic effects. Thanks to all these properties, the interest of the scientific community for it has grown.
Indeed, CBD is a great candidate for the management of neurological diseases. The purpose of our review is to summarize the in vitro and in vivo studies published in the last 15 years that describe the biochemical and molecular mechanisms underlying the effects of CBD and its therapeutic application in neurological diseases.
CBD exerts its neuroprotective effects through three G protein coupled-receptors (adenosine receptor subtype 2A, serotonin receptor subtype 1A and G protein-coupled receptor 55), one ligand-gated ion channel (transient receptor potential vanilloid channel-1) and one nuclear factor (peroxisome proliferator-activated receptor γ). Moreover, the therapeutical properties of CBD are also due to GABAergic modulation.
In conclusion, CBD, through multi-target mechanisms, represents a valid therapeutic tool for the management of epilepsy, Alzheimer’s disease, multiple sclerosis and Parkinson’s disease.”

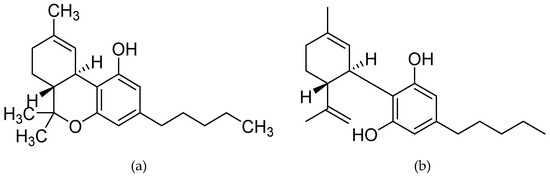
 “Δ9 -Tetrahydrocannabinol (THC), the main bioactive compound found in the plant Cannabis sativa, exerts its effects by activating cannabinoid receptors present in many neural cells.
“Δ9 -Tetrahydrocannabinol (THC), the main bioactive compound found in the plant Cannabis sativa, exerts its effects by activating cannabinoid receptors present in many neural cells. “Objectives
“Objectives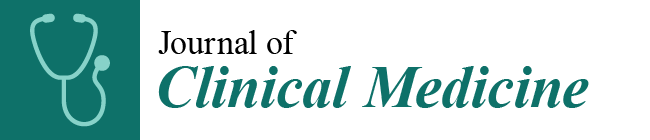 “Neurological disorders such as neurodegenerative diseases or traumatic brain injury are associated with cognitive, motor and behavioural changes that influence the quality of life of the patients. Although different therapeutic strategies have been developed and tried until now to decrease the neurological decline, no treatment has been found to cure these pathologies.
“Neurological disorders such as neurodegenerative diseases or traumatic brain injury are associated with cognitive, motor and behavioural changes that influence the quality of life of the patients. Although different therapeutic strategies have been developed and tried until now to decrease the neurological decline, no treatment has been found to cure these pathologies.
 “Objectives: To investigate the action of cannabinoids on spasticity and pain in secondary progressive multiple sclerosis, by means of neurophysiological indexes.
“Objectives: To investigate the action of cannabinoids on spasticity and pain in secondary progressive multiple sclerosis, by means of neurophysiological indexes. “Painful tonic spasm (PTS) is a common yet debilitating symptom in patients with neuromyelitis optica spectrum disorder (NMOSD), especially those with longitudinally extensive transverse myelitis. Although carbamazepine is an effective treatment, it poses the risk of severe adverse reactions, such as Steven-Johnson syndrome (SJS).
“Painful tonic spasm (PTS) is a common yet debilitating symptom in patients with neuromyelitis optica spectrum disorder (NMOSD), especially those with longitudinally extensive transverse myelitis. Although carbamazepine is an effective treatment, it poses the risk of severe adverse reactions, such as Steven-Johnson syndrome (SJS). “Cannabidiol (
“Cannabidiol ( “Moderate to severe spasticity is commonly reported in Multiple Sclerosis (MS) and its management is still a challenge. Cannabinoids were recently suggested as add-on therapy for the treatment of spasticity and chronic pain in MS but there is no conclusive scientific evidence on their safety, especially on cognition and over long periods.
“Moderate to severe spasticity is commonly reported in Multiple Sclerosis (MS) and its management is still a challenge. Cannabinoids were recently suggested as add-on therapy for the treatment of spasticity and chronic pain in MS but there is no conclusive scientific evidence on their safety, especially on cognition and over long periods. “Multiple sclerosis (MS) is an autoimmune demyelinating disease of the central nervous system, affecting ambulation even in people with only mild neurological signs. Patients with MS frequently experience spasticity, which contributes significantly to impair their motor functions, including ambulation, owing to muscle stiffness, spasms, and pain.
“Multiple sclerosis (MS) is an autoimmune demyelinating disease of the central nervous system, affecting ambulation even in people with only mild neurological signs. Patients with MS frequently experience spasticity, which contributes significantly to impair their motor functions, including ambulation, owing to muscle stiffness, spasms, and pain.