
“Cannabis preparations are gaining popularity among patients with various skin diseases. Due to the lack of scientific evidence, dermatologists remain cautious about their prescriptions. So far, only a few studies have been published about the effects of high-potency cannabis extracts on microorganisms (especially dermatophytes) causing skin problems that affect more than 25% of the worldwide population. Even though, the high-potency cannabis extracts prepared by cold extraction are mostly composed of non-psychoactive tetrahydrocannabinolic acid (THCA) and only low amount of THC, their use in topical treatment can be stigmatized. The in vitro antimicrobial and antifungal activity of two high potent cannabis strains extracted by three solvents traditionally or currently used by cannabis users (ethanol; EtOH, butane; BUT, dimethyl ether; DME) was investigated by broth dilution method. The chemical profile of cannabis was determined by high-performance liquid chromatography with ultraviolet detection and gas chromatography with mass spectrometer and flame ionization detector. The extraction methods significantly influenced chemical profile of extracts. The yield of EtOH extracts contained less cannabinoids and terpenes compared to BUT and DME ones. Most of the extracts was predominantly (>60%) composed of various cannabinoids, especially THCA. All of them demonstrated activity against 18 of the 19 microorganisms tested. The minimal inhibitory concentrations (MICs) of the extracts ranged from 4 to 256 μg/mL. In general, the bacteria were more susceptible to the extracts than dermatophytes. Due to the lower content of biologically active substances, the EtOH extracts were less effective against microorganisms. Cannabis extracts may be of value to treat dermatophytosis and other skin diseases caused by various microorganisms. Therefore, they could serve as an alternative or supportive treatment to commonly used antibiotics.”
https://pubmed.ncbi.nlm.nih.gov/36204633/
“Our research brought new evidence that cannabis extracts may be of value to treat dermatophytosis and other skin diseases caused by various microorganisms and showed that cannabis could serve as an alternative or supportive treatment to commonly used antibiotics.”
https://www.frontiersin.org/articles/10.3389/fmicb.2022.953092/full


 “UV phototherapy used in chronic skin diseases causes redox imbalance and pro-inflammatory reactions, especially in the case of unchanged skin cells.
“UV phototherapy used in chronic skin diseases causes redox imbalance and pro-inflammatory reactions, especially in the case of unchanged skin cells. “Cannabidiol (CBD), a natural occurring phytocannabinoid, is used extensively in consumer products ranging from foods to shampoos, topical oils and lotions.
“Cannabidiol (CBD), a natural occurring phytocannabinoid, is used extensively in consumer products ranging from foods to shampoos, topical oils and lotions. “Psoriasis is associated with increased production of reactive oxygen species which leads to oxidative stress.
“Psoriasis is associated with increased production of reactive oxygen species which leads to oxidative stress.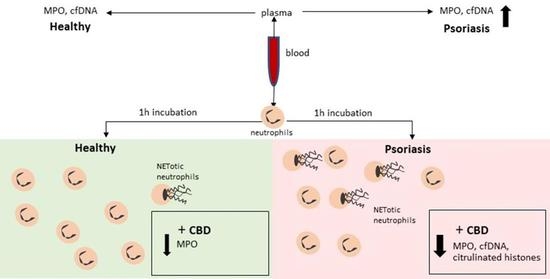
 “Psoriasis is a chronic inflammatory skin disease characterized by dysregulated keratinocyte differentiation, but oxidative stress also plays an important role in the pathogenesis of this disease.
“Psoriasis is a chronic inflammatory skin disease characterized by dysregulated keratinocyte differentiation, but oxidative stress also plays an important role in the pathogenesis of this disease. “The legalisation of
“The legalisation of  “Cannabinoids are increasingly-used substances in the treatment of chronic pain, some neuropsychiatric disorders and more recently, skin disorders with an inflammatory component.
“Cannabinoids are increasingly-used substances in the treatment of chronic pain, some neuropsychiatric disorders and more recently, skin disorders with an inflammatory component.