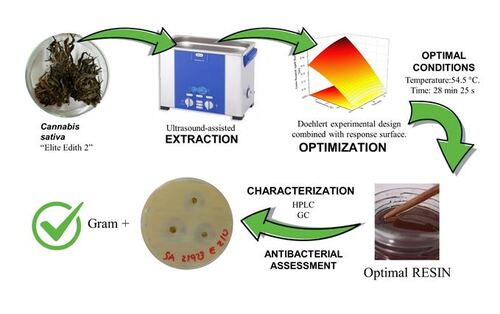
“Cannabis sativa yields a wide range of bioactive compounds, including terpenes, flavonoids, and cannabinoids.
Tetrahydrocannabinolic acid (THCA), cannabidiolic acid (CBDA), cannabigerolic acid (CBGA), and cannabichromenic acid (CBCA) are the acidic biosynthetic precursors of the neutral cannabinoids Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD), which have been the subject of much research.
This review examines the biosynthesis, decarboxylation, molecular pharmacology, and therapeutic significance of acidic cannabinoids, intending to address a significant knowledge gap. Peer-reviewed literature from major scientific databases was used in a systematic narrative review with an emphasis on investigations of acidic cannabinoid chemistry, pharmacology, pharmacokinetics, and disease-specific applications.
According to the reviewed data, acidic cannabinoids exhibit unique biological activities that distinguish them from their neutral counterparts. These include neuroprotective, anti-inflammatory, anticonvulsant, and anti-proliferative actions, which are mediated by molecular targets such as serotonin 5-HT1A receptors, cyclooxygenase-2 (COX-2), transient receptor potential (TRP) channels, and peroxisome proliferator-activated receptor-γ (PPARγ).
Acidic cannabinoids are more appealing for therapeutic usage in children and the elderly, considering that they are not intoxicating like THC; however, this distinction applies primarily to non‑heated consumption. Chemical instability, low bioavailability, and a dearth of controlled human trials impede clinical translation despite their potential.
According to the findings, acidic cannabinoids are an underutilized yet potentially valuable class of precision medicines.
In this study, we outline existing understanding on acidic cannabinoids, discuss their production and transformation, and identify research needs that could influence cannabis science research.”
https://pubmed.ncbi.nlm.nih.gov/41545891
https://link.springer.com/article/10.1186/s42238-026-00387-y
“Anti-Cancer Potential of Cannabinoids, Terpenes, and Flavonoids Present in Cannabis”
https://pmc.ncbi.nlm.nih.gov/articles/PMC7409346