 “Decline in cognitive performance, an aspect of the normal aging process, is influenced by the endocannabinoid system (ECS). Cannabinoid receptor 1 (CB1) signaling diminishes with advancing age in specific brain regions that regulate learning and memory and abolishing CB1 receptor signaling accelerates cognitive aging in mice.
“Decline in cognitive performance, an aspect of the normal aging process, is influenced by the endocannabinoid system (ECS). Cannabinoid receptor 1 (CB1) signaling diminishes with advancing age in specific brain regions that regulate learning and memory and abolishing CB1 receptor signaling accelerates cognitive aging in mice.
We recently demonstrated that prolonged exposure to low dose (3 mg/kg/day) Δ9-tetrahydrocannabinol (THC) improved the cognitive performances in old mice on par with young untreated mice. Here we investigated the potential influence of cannabidiol (CBD) on this THC effect, because preclinical and clinical studies indicate that the combination of THC and CBD often exhibits an enhanced therapeutic effect compared to THC alone.
We first tested the effectiveness of a lower dose (1 mg/kg/day) THC, and then the efficacy of the combination of THC and CBD in 1:1 ratio, same as in the clinically approved medicine Sativex®. Our findings reveal that a 1 mg/kg/day THC dose still effectively improved spatial learning in aged mice. However, a 1:1 combination of THC and CBD failed to do so.
The presence of CBD induced temporal changes in THC metabolism ensuing in a transient elevation of blood THC levels. However, as CBD metabolizes, the inhibitory effect on THC metabolism was alleviated, causing a rapid clearance of THC. Thus, the beneficial effects of THC seemed to wane off more swiftly in the presence of CBD, due to these metabolic effects.
The findings indicate that THC-treatment alone is more efficient to improve spatial learning in aged mice than the 1:1 combination of THC and CBD.”
https://pubmed.ncbi.nlm.nih.gov/34526890/
“In conclusion, our observations indicate that 1 mg/kg/day THC dose is still effective in improving the spatial learning in aged mice. With regard to the efficacy, THC-alone has proved to be more efficient in improving spatial learning in aged mice than its 1:1 combination with CBD. However, the possibility of THC/CBD being efficient in other ratios or at the earliest time-points, like immediately after the treatment cease, cannot be negated. Possibly, reducing the dose of CBD may improve the efficacy of the THC/CBD combination.”
https://www.frontiersin.org/articles/10.3389/fnagi.2021.718850/full

 “Aged skeletal muscle undergoes metabolic and structural alterations eventually resulting in a loss of muscle strength and mass, i.e. age-related sarcopenia. Therefore, novel targets for muscle growth purposes in elderly are needed.
“Aged skeletal muscle undergoes metabolic and structural alterations eventually resulting in a loss of muscle strength and mass, i.e. age-related sarcopenia. Therefore, novel targets for muscle growth purposes in elderly are needed.  “”Medicinal cannabis” is defined as the use of cannabis-based products for the treatment of an illness. Investigations of cannabis compounds in psychiatric and neurological illnesses primarily focus on the major cannabinoids, cannabidiol (CBD) and Δ
“”Medicinal cannabis” is defined as the use of cannabis-based products for the treatment of an illness. Investigations of cannabis compounds in psychiatric and neurological illnesses primarily focus on the major cannabinoids, cannabidiol (CBD) and Δ “The Endocannabinoid System (ECS) is primarily responsible for maintaining homeostasis, a balance in internal environment (temperature, mood, and immune system) and energy input and output in living, biological systems.
“The Endocannabinoid System (ECS) is primarily responsible for maintaining homeostasis, a balance in internal environment (temperature, mood, and immune system) and energy input and output in living, biological systems.  “Prostate cancer is the second most frequently occurring cancer diagnosed among males. Recent preclinical evidence implicates cannabinoids as powerful regulators of cell growth and differentiation. In this review, we focused on studies that demonstrated anticancer effects of cannabinoids and their possible mechanisms of action in prostate cancer. Besides the palliative effects of cannabinoids, research from the past two decades has demonstrated their promising potential as antitumor agents in a wide variety of cancers. This analysis may provide pharmacological insights into the selection of specific cannabinoids for the development of antitumor drugs for the treatment of prostate cancer.”
“Prostate cancer is the second most frequently occurring cancer diagnosed among males. Recent preclinical evidence implicates cannabinoids as powerful regulators of cell growth and differentiation. In this review, we focused on studies that demonstrated anticancer effects of cannabinoids and their possible mechanisms of action in prostate cancer. Besides the palliative effects of cannabinoids, research from the past two decades has demonstrated their promising potential as antitumor agents in a wide variety of cancers. This analysis may provide pharmacological insights into the selection of specific cannabinoids for the development of antitumor drugs for the treatment of prostate cancer.”
 “Colic is a common digestive disorder in horses and one of the most urgent problems in equine medicine. A growing body of literature has indicated that the activation of cannabinoid receptors could exert beneficial effects on gastrointestinal inflammation and visceral hypersensitivity.
“Colic is a common digestive disorder in horses and one of the most urgent problems in equine medicine. A growing body of literature has indicated that the activation of cannabinoid receptors could exert beneficial effects on gastrointestinal inflammation and visceral hypersensitivity.  “Studies investigating the psychosomatic effects of social isolation in animals have shown that one of the physiologic system that gets disrupted by this environment-affective change is the Endocannabinoid System. As the levels of endocannabinoids change in limbic areas and prefrontal cortex during stressful times, so is the subject more prone to fearful and negative thoughts and aggressive behavior. The interplay of social isolation on the hypothalamic-pituitary-adrenal axis and cannabinoid tone triggers a vicious cycle which further impairs the natural body’s homeostatic neuroendocrine levels and provokes a series of risk factors for developing health complications. In this paper, we explore the psychosomatic impact of prolonged quarantine in healthy individuals, and propose management and coping strategies that may improve endocannabinoid tone, such as integration of probiotics, cannabidiol, meditation, and physical exercise interventions with the aim of supporting interpersonal, individual, and professional adherence with COVID-19 emergency public measures whilst minimizing their psycho-physical impact.”
“Studies investigating the psychosomatic effects of social isolation in animals have shown that one of the physiologic system that gets disrupted by this environment-affective change is the Endocannabinoid System. As the levels of endocannabinoids change in limbic areas and prefrontal cortex during stressful times, so is the subject more prone to fearful and negative thoughts and aggressive behavior. The interplay of social isolation on the hypothalamic-pituitary-adrenal axis and cannabinoid tone triggers a vicious cycle which further impairs the natural body’s homeostatic neuroendocrine levels and provokes a series of risk factors for developing health complications. In this paper, we explore the psychosomatic impact of prolonged quarantine in healthy individuals, and propose management and coping strategies that may improve endocannabinoid tone, such as integration of probiotics, cannabidiol, meditation, and physical exercise interventions with the aim of supporting interpersonal, individual, and professional adherence with COVID-19 emergency public measures whilst minimizing their psycho-physical impact.”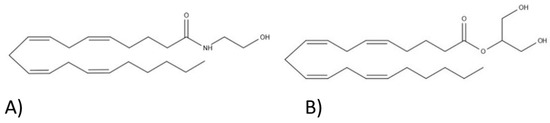
 “The Cannabis sativa plant has been used medicinally and recreationally for thousands of years, but recently only relatively some of its constituents have been identified.
“The Cannabis sativa plant has been used medicinally and recreationally for thousands of years, but recently only relatively some of its constituents have been identified.