 “Memantine and marijuana smoking have been previously found to inhibit tremor in parkinsonian patients, however, the observed effects were relatively weak. The tremorolytic efficacy of memantine and cannabinoid co-administration is unstudied.
“Memantine and marijuana smoking have been previously found to inhibit tremor in parkinsonian patients, however, the observed effects were relatively weak. The tremorolytic efficacy of memantine and cannabinoid co-administration is unstudied.
This work aimed to evaluate antitremor activity of memantine-Δ9 -tetrahydrocannabinol combination; additionally, the involvement of some neuroanatomical structures in the regulation of the combination effect was evaluated.
EXPERIMENTAL APPROACH:
Haloperidol-induced tremulous jaw movements in rats were used as a model of parkinsonian-like tremor. To evaluate the role of central receptor systems in the drug effect, receptor-targeting agents were administered locally into certain brain areas.
KEY RESULTS:
Memantine and Δ9 -tetrahydrocannabinol alone were without effect, however, co-administration of the drugs significantly decreased number of haloperidol-induced jaw movements. The antitremor activity of the combination was antagonized (i) by injections of L-glutamate into the dorsal striatum, entopeduncular nucleus, substantia nigra pars reticulata, globus pallidus, supratrigeminal and trigeminal motor nuclei but not into the subthalamic and cuneiform nuclei; (ii) by injections of CGS 21680 into the ventrolateral striatum; (iii) by injections of bicuculline into the rostral part of the parvicellular reticular nucleus.
CONCLUSION AND IMPLICATIONS:
Memantine and Δ9 -tetrahydrocannabinol supra-additively inhibit haloperidol-induced tremulous jaw movements. Apparently, the co-administration of the drugs might be a new approach to the treatment of tremor. The presented results identify brain areas influencing parkinsonian-like tremor in rats; these data can help advance the development of novel treatments for repetitive involuntary movements.”
https://www.ncbi.nlm.nih.gov/pubmed/31696510
https://bpspubs.onlinelibrary.wiley.com/doi/abs/10.1111/bph.14914
“Memantine is a prescription drug used to treat moderate to severe confusion (dementia) related to Alzheimer’s disease. Memantine is available under the following different brand names: Namenda XR, and Namenda.” https://www.rxlist.com/consumer_memantine_namenda/drugs-condition.htm

 “For persons living with chronic conditions, health-related quality of life (HRQoL) symptoms, such as pain, anxiety, depression, and insomnia, often interact and mutually reinforce one another.
“For persons living with chronic conditions, health-related quality of life (HRQoL) symptoms, such as pain, anxiety, depression, and insomnia, often interact and mutually reinforce one another. “L-dopa induced dyskinesia (LID) is a debilitating side-effect of the primary treatment used in Parkinson’s disease (PD), l-dopa. Here we investigate the effect of HU-308, a
“L-dopa induced dyskinesia (LID) is a debilitating side-effect of the primary treatment used in Parkinson’s disease (PD), l-dopa. Here we investigate the effect of HU-308, a  “Prostate cancer patients receiving androgen-deprivation therapy (ADT) often experience a combination of disease symptoms and treatment side effects. The therapeutic use of
“Prostate cancer patients receiving androgen-deprivation therapy (ADT) often experience a combination of disease symptoms and treatment side effects. The therapeutic use of  “The CB1 receptor mediates the central nervous system response to cannabinoids, and is a drug target for pain, anxiety and seizures.
“The CB1 receptor mediates the central nervous system response to cannabinoids, and is a drug target for pain, anxiety and seizures. “Bone cancer pain (BCP) is a severe complication of advanced bone cancer.
“Bone cancer pain (BCP) is a severe complication of advanced bone cancer. “WIN55,212-2 (WIN) is a synthetic agonist of
“WIN55,212-2 (WIN) is a synthetic agonist of 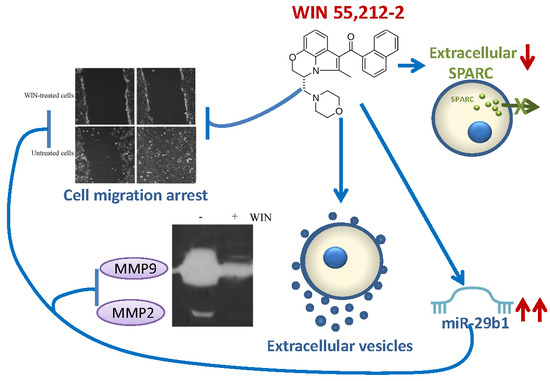
 “The symptomatic treatment of myotonia and myalgia in patients with dystrophic and non-dystrophic myotonias is often not satisfactory.
“The symptomatic treatment of myotonia and myalgia in patients with dystrophic and non-dystrophic myotonias is often not satisfactory.
 “Medical
“Medical