“Background/Objectives: Wound-related pain is a common, yet inadequately managed condition, and new therapeutic strategies are warranted. Limited data suggests that phytocannabinoids and cannabis may alleviate wound-related pain; however, further studies are required. This study investigated the effects of systemic administration of cannabidiol (CBD) on nociceptive behaviour following dorsum incision and on the endocannabinoid system.
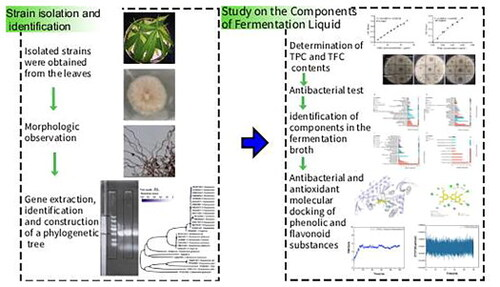
Methods: Male Sprague-Dawley rats (150-200 g on arrival, n = 9/group) underwent a 1.2 cm incision on the hairy skin of the dorsum or sham procedure. Back and hind paw mechanical withdrawal thresholds were assessed at baseline and post-surgery/sham days (PSDs) 1, 4, 7, and 8 using manual and electronic von Frey tests, respectively. On PSD 8, the effect of a single acute administration of CBD (3, 10, or 30 mg/kg, i.p.) on mechanical hypersensitivity in the dorsum and hind paws was assessed. The levels of endocannabinoids and N-acylethanolamines in the plasma and discrete brain regions following CBD administration were analysed.
Results: Robust mechanical hypersensitivity was evident in the dorsum and hind paws following the incision. CBD (3 mg/kg) partially attenuated primary mechanical hypersensitivity in the dorsum, in a site- and dose-specific manner. CBD had no effect on secondary mechanical hypersensitivity. CBD did not alter the levels of endocannabinoids or N-acylethanolamines, but in rats that received CBD (3 mg/kg), levels of 2-AG were lower in the contralateral amygdala and levels of AEA were higher in the contralateral lumbar spinal cord, compared to the ipsilateral sides.
Conclusions: These data provide evidence for antinociceptive effects of CBD in a model of incisional wound-related pain. Further research on CBD’s mechanism(s) of action is warranted. The potential antinociceptive effects of other phytocannabinoids in this model should also be investigated.”
https://pubmed.ncbi.nlm.nih.gov/41599645
“Cannabidiol (CBD) is a phytocannabinoid found in Cannabis sativa L.”
“These results indicate dose- and site-specific antinociceptive effects of CBD in a rat model of incisional wound-related pain, providing preclinical evidence to support the contention that CBD may have therapeutic potential for alleviating incisional wound-related pain.”
“These results also indicate that investigation of the potential antinociceptive effects of other phytocannabinoids in this model of incisional wound-related pain is warranted.”
https://www.mdpi.com/1424-8247/19/1/43