“Cannabidiol is a Cannabis-derived non-psychotropic compound that exerts a plethora of pharmacological actions, including anti-inflammatory, neuroprotective and antitumour effects, with potential therapeutic interest. However, the actions of cannabidiol in the digestive tract are largely unexplored. In the present study, we investigated the effect of cannabidiol on intestinal motility in normal (control) mice and in mice with intestinal inflammation.”
“Cannabidiol selectively reduces croton oil-induced hypermotility in mice in vivo and this effect involves cannabinoid CB1 receptors and FAAH. In view of its low toxicity in humans, cannabidiol may represent a good candidate to normalize motility in patients with inflammatory bowel disease.”
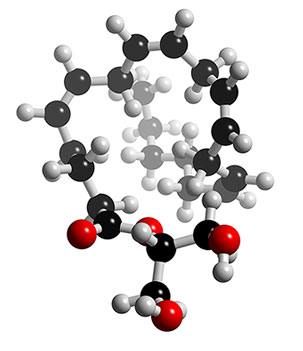
“The plant Cannabis sativa contains more than 60 terpenophenolic compounds, named phytocannabinoids. The best-studied phytocannabinoid is Δ9-tetrahydrocannabinol, which binds specific G-protein-coupled receptors, named cannabinoid (CB1 and CB2) receptors. The well-known psychotropic effects of Δ9-tetrahydrocannabinol, which are largely mediated by activation of brain cannabinoid CB1 receptors, have always raised a number of clinical and ethical problems. Therefore, a valid therapeutic alternative may be the use of non-psychotropic phytocannabinoids, including cannabidiol (CBD). CBD, unlike Δ9-tetrahydrocannabinol, has very low affinity for both cannabinoid CB1 and CB2 receptors, although it has been proposed that CBD may modulate endocannabinoid function through its ability to inhibit the hydrolysis of anandamide and to act as a transient receptor potential vanilloid 1 agonist. CBD is a major component of Sativex, a preparation of cannabinoids, which has been approved by Health Canada for the treatment of neuropathic pain in multiple sclerosis.”
“The pharmacological profile of CBD has been recently reviewed. Briefly stated, CBD has been shown to exert (1) antioxidant, neuroprotective and antiproliferative actions in cultured cells and (2) anti-anxiety, hypnotic, anticonvulsant, neuroprotective, antinausea, anti-ischaemic, anticancer and notably anti-inflammatory effects in rodents in vivo. The anti-inflammatory effects of CBD have been demonstrated in both acute and chronic experimental models of inflammation, that is, paw oedema and arthritis.”
“In conclusion, we have shown that the marijuana component CBD normalize intestinal motility in an experimental model of ileitis. In vitro results showed antispasmodic actions of CBD on intestinal ileal segments. The inhibitory effect of CBD involves, at least in vivo, cannabinoid CB1 receptors and FAAH. In view of its safety records in humans (an average daily dose of about 700 mg/day for 6 weeks was found to be non-toxic, relative to placebo, in clinical trials; and because CBD reduced motility during inflammation and not in physiological conditions, CBD might be considered as a good candidate to be clinically evaluated for the treatment of hypermotility associated with inflammatory bowel disease.”
mg/day for 6 weeks was found to be non-toxic, relative to placebo, in clinical trials; and because CBD reduced motility during inflammation and not in physiological conditions, CBD might be considered as a good candidate to be clinically evaluated for the treatment of hypermotility associated with inflammatory bowel disease.”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2451037/

 mg/day for 6 weeks was found to be non-toxic, relative to placebo, in clinical trials; and because CBD reduced motility during inflammation and not in physiological conditions, CBD might be considered as a good candidate to be clinically evaluated for the treatment of hypermotility associated with inflammatory bowel disease.”
mg/day for 6 weeks was found to be non-toxic, relative to placebo, in clinical trials; and because CBD reduced motility during inflammation and not in physiological conditions, CBD might be considered as a good candidate to be clinically evaluated for the treatment of hypermotility associated with inflammatory bowel disease.”