 “Alzheimer’s disease (AD), the leading cause of dementia in the elderly, is a neurodegenerative disorder marked by progressive impairment of cognitive ability. Patients with AD display neuropathological lesions including senile plaques, neurofibrillary tangles, and neuronal loss.
“Alzheimer’s disease (AD), the leading cause of dementia in the elderly, is a neurodegenerative disorder marked by progressive impairment of cognitive ability. Patients with AD display neuropathological lesions including senile plaques, neurofibrillary tangles, and neuronal loss.
There are no disease-modifying drugs currently available. With the number of affected individuals increasing dramatically throughout the world, there is obvious urgent need for effective treatment strategy for AD.
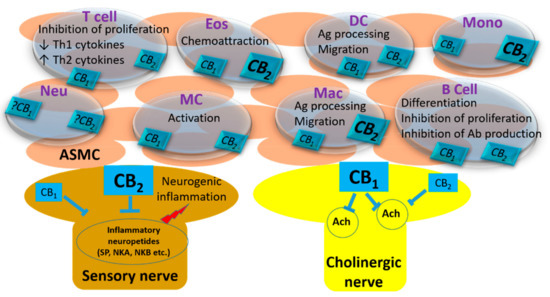
The multifactorial nature of AD encouraged the development of multifunctional compounds, able to interact with several putative targets. Here, we have evaluated the effects of two in-house designed cannabinoid receptors (CB) agonists showing inhibitory actions on β-secretase-1 (BACE-1) (NP137) and BACE-1/butyrylcholinesterase (BuChE) (NP148), on cellular models of AD, including immortalized lymphocytes from late-onset AD patients.
We report here that NP137 and NP148 showed neuroprotective effects in amyloid-β-treated primary cortical neurons, and NP137 in particular rescued the cognitive deficit of TgAPP mice. The latter compound was able to blunt the abnormal cell response to serum addition or withdrawal of lymphoblasts derived from AD patients.
It is suggested that NP137 could be a good drug candidate for future treatment of AD.”
https://www.ncbi.nlm.nih.gov/pubmed/31898159
https://link.springer.com/article/10.1007%2Fs12035-019-01813-4
“The ideal treatment for AD should be able to modulate the disease through multiple mechanisms rather than targeting a single dysregulated pathway.” http://www.ncbi.nlm.nih.gov/pubmed/25147120
“These sets of data strongly suggest that THC could be a potential therapeutic treatment option for Alzheimer’s disease through multiple functions and pathways.” http://www.ncbi.nlm.nih.gov/pubmed/25024327
“In fact, exogenous and endogenous cannabinoids seem to be able to modulate multiple processes in AD” http://www.ncbi.nlm.nih.gov/pubmed/25147120
“Our results indicate that cannabinoid receptors are important in the pathology of AD and that cannabinoids succeed in preventing the neurodegenerative process occurring in the disease.” http://www.ncbi.nlm.nih.gov/pubmed/15728830
“Based on the complex pathology of AD, a preventative, multimodal drug approach targeting a combination of pathological AD symptoms appears ideal. Importantly, cannabinoids show anti-inflammatory, neuroprotective and antioxidant properties and have immunosuppressive effects.” http://www.ncbi.nlm.nih.gov/pubmed/22448595
“CBD treatment would be in line with preventative, multimodal drug strategies targeting a combination of pathological symptoms, which might be ideal for AD therapy.” http://www.ncbi.nlm.nih.gov/pubmed/27471947

 “In traditional medicine, Cannabis sativa has been prescribed for a variety of diseases. Today, the plant is largely known for its recreational purpose, but it may find a way back to what it was originally known for: a herbal remedy. Most of the plant’s ingredients, such as Δ-tetrahydrocannabinol,
“In traditional medicine, Cannabis sativa has been prescribed for a variety of diseases. Today, the plant is largely known for its recreational purpose, but it may find a way back to what it was originally known for: a herbal remedy. Most of the plant’s ingredients, such as Δ-tetrahydrocannabinol,  “Neuropathic pain associated with nucleoside reverse transcriptase inhibitors (NRTIs), therapeutic agents for human immunodeficiency virus (HIV), responds poorly to available drugs.
“Neuropathic pain associated with nucleoside reverse transcriptase inhibitors (NRTIs), therapeutic agents for human immunodeficiency virus (HIV), responds poorly to available drugs. “The butyl homologues of Δ9-tetrahydrocannabinol, Δ9-tetrahydrocannabutol (Δ9-THCB), and
“The butyl homologues of Δ9-tetrahydrocannabinol, Δ9-tetrahydrocannabutol (Δ9-THCB), and 
 “Chronic stress is depressogenic by altering neurotrophic and neuroinflammatory environments of the organism. The endocannabinoid system controls cognitive and emotional responses related with stress through the interaction with endocannabinoid receptors. β-Caryophyllene (BCP) is a CB2 agonist that exhibited anti-inflammatory, analgesic effects but minimal psychoactive effects. To test if BCP exhibits antidepressant-like action, animals were chronically restrained with additional stressors for 28 days, and BCP (25, 50, 100 mg/kg) was intraperitoneally injected once a day during the stress inflicting period. Then despair related behaviors and hippocampal expression of neurotrophic, inflammatory and
“Chronic stress is depressogenic by altering neurotrophic and neuroinflammatory environments of the organism. The endocannabinoid system controls cognitive and emotional responses related with stress through the interaction with endocannabinoid receptors. β-Caryophyllene (BCP) is a CB2 agonist that exhibited anti-inflammatory, analgesic effects but minimal psychoactive effects. To test if BCP exhibits antidepressant-like action, animals were chronically restrained with additional stressors for 28 days, and BCP (25, 50, 100 mg/kg) was intraperitoneally injected once a day during the stress inflicting period. Then despair related behaviors and hippocampal expression of neurotrophic, inflammatory and  “Beta-caryophyllene is an odoriferous bicyclic sesquiterpene found in various herbs and spices.
“Beta-caryophyllene is an odoriferous bicyclic sesquiterpene found in various herbs and spices. “As a library of cannabinoid (CB) derivatives with (-)-trans–
“As a library of cannabinoid (CB) derivatives with (-)-trans– “Epilepsy is a neurological disorder that affects approximately 50 million people worldwide.
“Epilepsy is a neurological disorder that affects approximately 50 million people worldwide.