 “Cannabinoids are increasingly-used substances in the treatment of chronic pain, some neuropsychiatric disorders and more recently, skin disorders with an inflammatory component.
“Cannabinoids are increasingly-used substances in the treatment of chronic pain, some neuropsychiatric disorders and more recently, skin disorders with an inflammatory component.
This paper aims to detail and clarify the complex workings of cannabinoids in the molecular setting of the main dermatological inflammatory diseases, and their interactions with other substances with emerging applications in the treatment of these conditions. Also, the potential role of cannabinoids as antitumoral drugs is explored in relation to the inflammatory component of skin cancer.
In vivo and in vitro studies that employed either phyto-, endo-, or synthetic cannabinoids were considered in this paper. Cannabinoids are regarded with growing interest as eligible drugs in the treatment of skin inflammatory conditions, with potential anticancer effects, and the readiness in monitoring of effects and the facility of topical application may contribute to the growing support of the use of these substances.
Despite the promising early results, further controlled human studies are required to establish the definitive role of these products in the pathophysiology of skin inflammation and their usefulness in the clinical setting.”
https://www.ncbi.nlm.nih.gov/pubmed/32033005
https://www.mdpi.com/1420-3049/25/3/652
“Cannabinoid Signaling in the Skin: Therapeutic Potential of the “C(ut)annabinoid” System” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6429381/

 “Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.
“Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.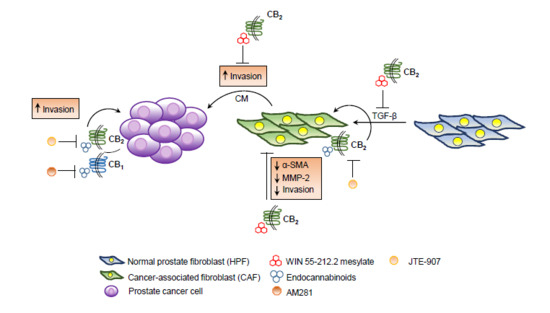
 “The monocyclic 1,4-benzoquinone, HU-331, the direct oxidation product of
“The monocyclic 1,4-benzoquinone, HU-331, the direct oxidation product of  “According to recent studies,
“According to recent studies, 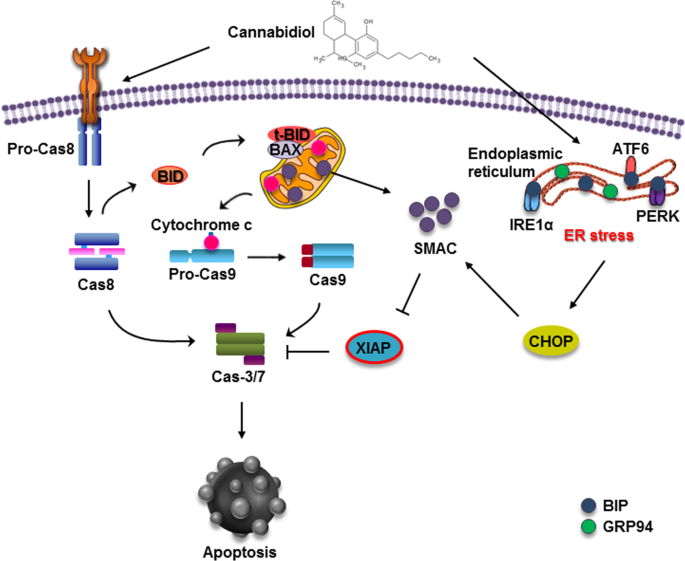
 “The anticancer effects of the omega-3 long chain polyunsaturated fatty acids (LCPUFA), EPA and DHA may be due, at least in part, to conversion to their respective endocannabinoid derivatives, eicosapentaenoyl-ethanolamine (EPEA) and docosahexaenoyl-ethanolamine (DHEA).
“The anticancer effects of the omega-3 long chain polyunsaturated fatty acids (LCPUFA), EPA and DHA may be due, at least in part, to conversion to their respective endocannabinoid derivatives, eicosapentaenoyl-ethanolamine (EPEA) and docosahexaenoyl-ethanolamine (DHEA). “Cannabinoids exhibit anti-inflammatory and antitumorigenic properties.
“Cannabinoids exhibit anti-inflammatory and antitumorigenic properties. “Anticancer properties of non-psychoactive cannabinoid
“Anticancer properties of non-psychoactive cannabinoid  “Cancer patients experience multiple symptoms throughout their illness, and some report benefit from the use of cannabis. There are concerns that many patients are accessing products inappropriate for their situation and potentially putting themselves at risk.
“Cancer patients experience multiple symptoms throughout their illness, and some report benefit from the use of cannabis. There are concerns that many patients are accessing products inappropriate for their situation and potentially putting themselves at risk. “Ovarian cancer, with over a 90% reoccurrence within 18 months of treatment, and approximately a 30% mortality rate after 5 years, is the leading cause of death in cases of gynaecological malignancies. Acquired resistance, and toxic side effects by clinically used agents are major challenges associated with current treatments, indicating the need for new approaches in ovarian cancer treatment.
“Ovarian cancer, with over a 90% reoccurrence within 18 months of treatment, and approximately a 30% mortality rate after 5 years, is the leading cause of death in cases of gynaecological malignancies. Acquired resistance, and toxic side effects by clinically used agents are major challenges associated with current treatments, indicating the need for new approaches in ovarian cancer treatment.