 “There is uncertainty regarding the appropriate dose of Cannabidiol (CBD) for childhood epilepsy.
“There is uncertainty regarding the appropriate dose of Cannabidiol (CBD) for childhood epilepsy.
We present the preliminary data of seven participants from the Cannabidiol in Children with Refractory Epileptic Encephalopathy (CARE-E) study.
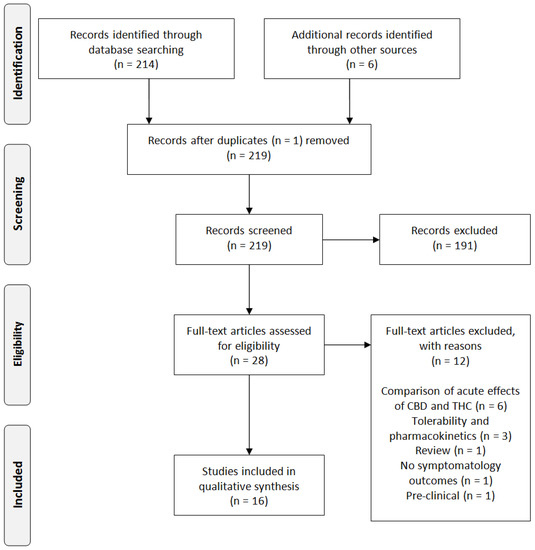
Methods: The study is an open-label, prospective, dose-escalation trial. Participants received escalating doses of a Cannabis Herbal Extract (CHE) preparation of 1:20 Δ9-tetrahydrocannabinol (THC): CBD up to 10-12 mg CBD/kg/day. Seizure frequency was monitored in daily logs, participants underwent regular electroencephalograms, and parents filled out modified Quality of Life in Childhood Epilepsy (QOLCE) and Side Effect rating scale questionnaires. Steady-state trough levels (Css, Min) of selected cannabinoids were quantified.
Results: All seven participants tolerated the CHE up to 10-12 mg CBD/kg/day and had improvements in seizure frequency and QOLCE scores. CSS, Min plasma levels for CBD, THC, and cannabichromene (CBC) showed dose-independent pharmacokinetics in all but one participant. CSS, Min CBD levels associated with a >50% reduction in seizures and seizure freedom were lower than those reported previously with purified CBD. In most patients, CSS, Min levels of THC remained lower than what would be expected to cause intoxication.
Conclusion: The preliminary data suggest an initial CBD target dose of 5-6 mg/kg/day when a 1:20 THC:CBD CHE is used. Possible non-linear pharmacokinetics of CBD and CBC needs investigation. The reduction in seizure frequency seen suggests improved seizure control when a whole plant CHE is used. Plasma THC levels suggest a low risk of THC intoxication when a 1:20 THC:CBD CHE is used in doses up to 12 mg/kg CBD/kg/day.”
https://www.ncbi.nlm.nih.gov/pubmed/31333569
https://www.frontiersin.org/articles/10.3389/fneur.2019.00716/full

 “The Cannabis plant has been used for many of years as a medicinal agent in the relief of pain and seizures. It contains approximately 540 natural compounds including more than 100 that have been identified as phytocannabinoids due to their shared chemical structure. The predominant psychotropic component is Δ9-tetrahydrocannabinol (Δ9-THC), while the major non-psychoactive ingredient is
“The Cannabis plant has been used for many of years as a medicinal agent in the relief of pain and seizures. It contains approximately 540 natural compounds including more than 100 that have been identified as phytocannabinoids due to their shared chemical structure. The predominant psychotropic component is Δ9-tetrahydrocannabinol (Δ9-THC), while the major non-psychoactive ingredient is 
 “Cannabidiol (CBD), a non-euphorigenic compound derived from
“Cannabidiol (CBD), a non-euphorigenic compound derived from  “Cognitive impairment is a major source of disability in schizophrenia and current antipsychotic drugs (APDs) have minimal efficacy for this symptom domain.
“Cognitive impairment is a major source of disability in schizophrenia and current antipsychotic drugs (APDs) have minimal efficacy for this symptom domain.
 “Herein, we report the antioxidant activity of
“Herein, we report the antioxidant activity of 
 “Currently, there are no approved pharmacotherapies for addiction to cocaine and other psychostimulant drugs. Several studies have proposed that
“Currently, there are no approved pharmacotherapies for addiction to cocaine and other psychostimulant drugs. Several studies have proposed that