 “Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.
“Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.
Recent evidence describes the use of cannabinoids in the treatment of fibromyalgia.
This study provides a systematic, thorough review of the evidence alongside a review of the seminal data regarding the pathophysiology, diagnosis, and current treatment options.
Fibromyalgia is characterized by widespread chronic pain, fatigue, and depressive episodes without an organic diagnosis, which may be prevalent in up to 10% of the population and carries a significant cost in healthcare utilization, morbidity, a reduced quality of life, and productivity. It is frequently associated with psychiatric comorbidities. The diagnosis is clinical and usually prolonged, and diagnostic criteria continue to evolve. Some therapies have been previously described, including neuropathic medications, milnacipran, and antidepressants. Despite some level of efficacy, only physical exercise has strong evidence to support it.
Cannabis has been used historically to treat different pain conditions since ancient times.
Recent advances allowed for the isolation of the active substances in cannabis and the production of cannabinoid products that are nearly devoid of psychoactive influence and provide pain relief and alleviation of other symptoms. Many of these, as well as cannabis itself, are approved for use in chronic pain conditions.
Evidence supporting cannabis in chronic pain conditions is plentiful; however, in fibromyalgia, they are mostly limited. Only a handful of randomized trials exists, and their objectivity has been questioned. However, many retrospective trials and patient surveys suggest the significant alleviation of pain, improvement in sleep, and abatement of associated symptoms.
Evidence supporting the use of cannabis in chronic pain and specifically in fibromyalgia is being gathered as the use of cannabis increases with current global trends. While the current evidence is still limited, emerging data do suggest a positive effect of cannabis in fibromyalgia.
Cannabis use is not without risks, including psychiatric, cognitive, and developmental as well as the risks of addiction. As such, clinical judgment is warranted to weigh these risks and prescribe to patients who are more likely to benefit from this treatment. Further research is required to define appropriate patient selection and treatment regimens.”
https://pubmed.ncbi.nlm.nih.gov/33004171/
https://www.sciencedirect.com/science/article/pii/S1521689620300781?via%3Dihub
 “These data support the notion that CBD and CBDV act as functional partial agonists on dopamine D2-like receptors in vivo.
“These data support the notion that CBD and CBDV act as functional partial agonists on dopamine D2-like receptors in vivo.
 “In this proof-of-concept study, the antioxidant activity of phytocannabinoids, namely cannabidiol (CBD) and Δ9- tetrahydrocannabinol (THC), were investigated using an in vitro system of differentiated human neuronal SY-SH5Y cells.
“In this proof-of-concept study, the antioxidant activity of phytocannabinoids, namely cannabidiol (CBD) and Δ9- tetrahydrocannabinol (THC), were investigated using an in vitro system of differentiated human neuronal SY-SH5Y cells.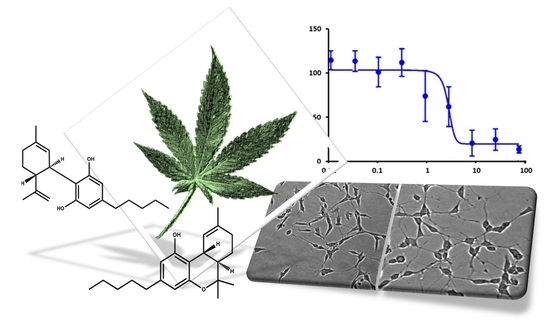
 “UV phototherapy used in chronic skin diseases causes redox imbalance and pro-inflammatory reactions, especially in the case of unchanged skin cells.
“UV phototherapy used in chronic skin diseases causes redox imbalance and pro-inflammatory reactions, especially in the case of unchanged skin cells. “This study evaluated the synergistic anti-cancer potential of cannabinoid combinations across the MDA-MB-231 and MCF-7 human breast cancer cell lines. Cannabinoids were combined and their synergistic interactions were evaluated using median effect analysis.
“This study evaluated the synergistic anti-cancer potential of cannabinoid combinations across the MDA-MB-231 and MCF-7 human breast cancer cell lines. Cannabinoids were combined and their synergistic interactions were evaluated using median effect analysis. “Considering lack of target-specific antiviral treatment and vaccination for COVID-19, it is absolutely exigent to have an effective therapeutic modality to reduce hospitalization and mortality rate as well as to improve COVID-19-infected patient outcomes.
“Considering lack of target-specific antiviral treatment and vaccination for COVID-19, it is absolutely exigent to have an effective therapeutic modality to reduce hospitalization and mortality rate as well as to improve COVID-19-infected patient outcomes. “Epilepsy is a chronic neurological disease characterized by recurrent epileptic seizures. Studies have shown the complexity of epileptogenesis and ictogenesis, in which immunological processes and epigenetic and structural changes in neuronal tissues have been identified as triggering epilepsy.
“Epilepsy is a chronic neurological disease characterized by recurrent epileptic seizures. Studies have shown the complexity of epileptogenesis and ictogenesis, in which immunological processes and epigenetic and structural changes in neuronal tissues have been identified as triggering epilepsy. “Anxiety disorders in young people are frequently comorbid with other mental disorders and respond unsatisfactorily to first-line treatment in many cases.
“Anxiety disorders in young people are frequently comorbid with other mental disorders and respond unsatisfactorily to first-line treatment in many cases. “Pharmaceutically purified oral cannabidiol (CBD) has been recently approved by the US Food and Drug Administration and European Medicines Agency as treatment of seizures associated with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS), which are severe and difficult-to-treat developmental and epileptic encephalopathies with onset in early childhood.
“Pharmaceutically purified oral cannabidiol (CBD) has been recently approved by the US Food and Drug Administration and European Medicines Agency as treatment of seizures associated with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS), which are severe and difficult-to-treat developmental and epileptic encephalopathies with onset in early childhood. “Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.
“Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.