 “Acute Respiratory Distress Syndrome (ARDS) is a life-threatening complication that can ensue following Staphylococcus aureus infection. The enterotoxin produced by these bacteria (SEB) acts as a superantigen thereby activating a large proportion of T cells leading to cytokine storm and severe lung injury.
“Acute Respiratory Distress Syndrome (ARDS) is a life-threatening complication that can ensue following Staphylococcus aureus infection. The enterotoxin produced by these bacteria (SEB) acts as a superantigen thereby activating a large proportion of T cells leading to cytokine storm and severe lung injury.
Δ9Tetrahydrocannabinol (THC), a psychoactive ingredient found in Cannabis sativa, has been shown to act as a potent anti-inflammatory agent. In the current study, we investigated the effect of THC treatment on SEB-induced ARDS in mice.
While exposure to SEB resulted in acute mortality, treatment with THC led to 100% survival of mice. THC treatment significantly suppressed the inflammatory cytokines, IFN-γ and TNF-α. Additionally, THC elevated the induction of regulatory T cells (Tregs) and their associated cytokines, IL-10 and TGF-β. Moreover, THC caused induction of Myeloid-Derived Suppressor Cells (MDSCs).
THC acted through CB2 receptor as pharmacological inhibitor of CB2 receptors blocked the anti-inflammatory effects. THC-treated mice showed significant alterations in the expression of miRNA (miRs) in the lung-infiltrated mononuclear cells (MNCs). Specifically, THC caused downregulation of let7a-5p which targeted SOCS1 and downregulation of miR-34-5p which caused increased expression of FoxP3, NOS1, and CSF1R.
Together, these data suggested that THC-mediated alterations in miR expression in the lungs may play a critical role in the induction of immunosuppressive Tregs and MDSCs as well as suppression of cytokine storm leading to attenuation of SEB-mediated lung injury.”
https://pubmed.ncbi.nlm.nih.gov/32612530/
“In summary, the current study suggests that treatment of mice with THC post-SEB challenge protects mice from SEB-mediated toxicity by inhibiting inflammation and ARDS through the modulation of miRs. Because SEB is a super antigen that drives cytokine storm, our studies suggest that THC is a potent anti-inflammatory agent that has the potential to be used as a therapeutic modality to treat SEB-induced ARDS.
It is of interest to note that a significant proportion of Coronavirus disease 2019 (COVID-19) patients come down with sepsis and ARDS accompanied by cytokine storm. ”
https://www.frontiersin.org/articles/10.3389/fphar.2020.00893/full

 “Like most modern molecular biology and natural product chemistry, understanding cannabinoid pharmacology centers around molecular interactions, in this case, between the cannabinoids and their putative targets, the G-protein coupled receptors (GPCRs) cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2). Understanding the complex structure and interplay between the partners in this molecular dance is required to understand the mechanism of action of synthetic, endogenous, and phytochemical cannabinoids. This review, with 91 references, surveys our understanding of the structural biology of the cannabinoids and their target receptors including both a critical comparison of the extant crystal structures and the computationally derived homology models, as well as an in-depth discussion about the binding modes of the major cannabinoids. The aim is to assist in situating structural biochemists, synthetic chemists, and molecular biologists who are new to the field of cannabis research.”
“Like most modern molecular biology and natural product chemistry, understanding cannabinoid pharmacology centers around molecular interactions, in this case, between the cannabinoids and their putative targets, the G-protein coupled receptors (GPCRs) cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2). Understanding the complex structure and interplay between the partners in this molecular dance is required to understand the mechanism of action of synthetic, endogenous, and phytochemical cannabinoids. This review, with 91 references, surveys our understanding of the structural biology of the cannabinoids and their target receptors including both a critical comparison of the extant crystal structures and the computationally derived homology models, as well as an in-depth discussion about the binding modes of the major cannabinoids. The aim is to assist in situating structural biochemists, synthetic chemists, and molecular biologists who are new to the field of cannabis research.” “Astrocytomas, the most prevalent primary brain tumors, can be divided by histology and malignancy levels into four following types: pilocytic astrocytoma (grade I), diffuse fibrillary astrocytoma (grade II), anaplastic astrocytoma (grade III), and glioblastoma multiforme (grade IV). For high grade astrocytomas (grade III and grade IV), blood vessels formation is considered as the most important property.
“Astrocytomas, the most prevalent primary brain tumors, can be divided by histology and malignancy levels into four following types: pilocytic astrocytoma (grade I), diffuse fibrillary astrocytoma (grade II), anaplastic astrocytoma (grade III), and glioblastoma multiforme (grade IV). For high grade astrocytomas (grade III and grade IV), blood vessels formation is considered as the most important property. “Acute Respiratory Distress Syndrome (ARDS) is a life-threatening complication that can ensue following Staphylococcus aureus infection. The enterotoxin produced by these bacteria (SEB) acts as a superantigen thereby activating a large proportion of T cells leading to cytokine storm and severe lung injury.
“Acute Respiratory Distress Syndrome (ARDS) is a life-threatening complication that can ensue following Staphylococcus aureus infection. The enterotoxin produced by these bacteria (SEB) acts as a superantigen thereby activating a large proportion of T cells leading to cytokine storm and severe lung injury. “The efficacy of cannabidiol (CBD) with and without concomitant clobazam (CLB) was evaluated in stratified analyses of four large randomized controlled trials, two in Lennox-Gastaut syndrome and two in Dravet syndrome.
“The efficacy of cannabidiol (CBD) with and without concomitant clobazam (CLB) was evaluated in stratified analyses of four large randomized controlled trials, two in Lennox-Gastaut syndrome and two in Dravet syndrome. “The Cannabis plant contains numerous components, including cannabinoids and other active molecules. The phyto-cannabinoid activity is mediated by the endocannabinoid system. Cannabinoids affect the nervous system and play significant roles in the regulation of the immune system.
“The Cannabis plant contains numerous components, including cannabinoids and other active molecules. The phyto-cannabinoid activity is mediated by the endocannabinoid system. Cannabinoids affect the nervous system and play significant roles in the regulation of the immune system.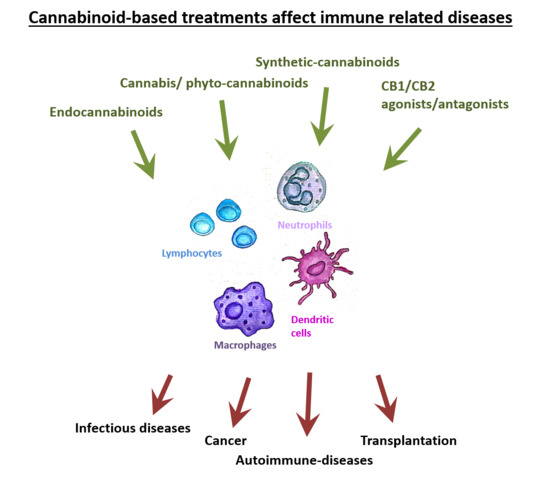
 “Painful tonic spasm (PTS) is a common yet debilitating symptom in patients with neuromyelitis optica spectrum disorder (NMOSD), especially those with longitudinally extensive transverse myelitis. Although carbamazepine is an effective treatment, it poses the risk of severe adverse reactions, such as Steven-Johnson syndrome (SJS).
“Painful tonic spasm (PTS) is a common yet debilitating symptom in patients with neuromyelitis optica spectrum disorder (NMOSD), especially those with longitudinally extensive transverse myelitis. Although carbamazepine is an effective treatment, it poses the risk of severe adverse reactions, such as Steven-Johnson syndrome (SJS). “The phosphatidylinositol 3-kinase (PI3K)/protein kinase B (PKB/Akt)/mechanistic target of rapamycin (mTOR) signaling pathway has been associated with several pathologies in the central nervous system (CNS), including epilepsy. There is evidence supporting the hypothesis that the PI3Kγ signaling pathway may mediate the powerful anticonvulsant properties associated with the cannabinoidergic system.
“The phosphatidylinositol 3-kinase (PI3K)/protein kinase B (PKB/Akt)/mechanistic target of rapamycin (mTOR) signaling pathway has been associated with several pathologies in the central nervous system (CNS), including epilepsy. There is evidence supporting the hypothesis that the PI3Kγ signaling pathway may mediate the powerful anticonvulsant properties associated with the cannabinoidergic system.