 “Gynaecological cancers can be primary neoplasms, originating either from the reproductive tract or the products of conception, or secondary neoplasms, representative of metastatic disease. For some of these cancers, the exact causes are unknown; however, it is recognised that the precise aetiopathogeneses for most are multifactorial and include exogenous (such as diet) and endogenous factors (such as genetic predisposition), which mutually interact in a complex manner.
“Gynaecological cancers can be primary neoplasms, originating either from the reproductive tract or the products of conception, or secondary neoplasms, representative of metastatic disease. For some of these cancers, the exact causes are unknown; however, it is recognised that the precise aetiopathogeneses for most are multifactorial and include exogenous (such as diet) and endogenous factors (such as genetic predisposition), which mutually interact in a complex manner.
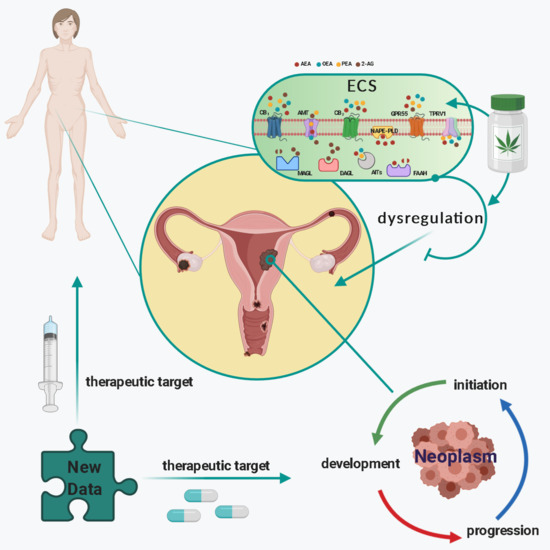
One factor that has been recognised to be involved in the pathogenesis and progression of gynaecological cancers is the endocannabinoid system (ECS). The ECS consists of endocannabinoids (bioactive lipids), their receptors, and metabolic enzymes responsible for their synthesis and degradation. In this review, the impact of plant-derived (Cannabis species) cannabinoids and endocannabinoids on gynaecological cancers will be discussed within the context of the complexity of the proteins that bind, transport, and metabolise these compounds in reproductive and other tissues. In particular, the potential of endocannabinoids, their receptors, and metabolic enzymes as biomarkers of specific cancers, such as those of the endometrium, will be addressed. Additionally, the therapeutic potential of targeting selected elements of the ECS as new action points for the development of innovative drugs will be presented.”
https://pubmed.ncbi.nlm.nih.gov/33375539/
“Cancers of the female reproductive system are common and are responsible for a large number of deaths in women. The exact reasons why some of these cancers occur are unknown. It is, however, known that for most of these cancers, several factors interact for them to happen. These interactions involve factors external and internal to the woman. An understanding of some of the internal factors involved in how these cancers arise will not only help drive preventive strategies, but will speed the development of new treatment approaches.
The endocannabinoid system is a family including chemicals (known as endocannabinoids) produced in the body that are similar to those derived from the cannabis plant. This system, which is widely distributed in the body, has been shown to be involved in various functions. Its disruption has been shown to lead to various diseases, one of which is cancer. In this review, we summarise current knowledge of this system, its various constituents, and how they are involved in reproductive events and their pathologies, especially cancers. Furthermore, we discuss the role of the endocannabinoid system in these cancers and how targeting it could lead to new approaches to diagnosis and treatment of cancers of the female reproductive system.”
https://www.mdpi.com/2072-6694/13/1/37
 “Cannabidiol (CBD) is one of the most popular emerging plant extracts that is being investigated for its wide range of potential health benefits.
“Cannabidiol (CBD) is one of the most popular emerging plant extracts that is being investigated for its wide range of potential health benefits.
 “Objective: The opioid epidemic continues to claim thousands of lives every year without an effective strategy useful in mitigating mortality. The use of medical cannabis has been proposed as a potential strategy to decrease opioid usage. The objective of this study was to determine how the use of medical cannabis affects prescribed opioid usage in chronic pain patients.
“Objective: The opioid epidemic continues to claim thousands of lives every year without an effective strategy useful in mitigating mortality. The use of medical cannabis has been proposed as a potential strategy to decrease opioid usage. The objective of this study was to determine how the use of medical cannabis affects prescribed opioid usage in chronic pain patients. “Background: The ongoing opioid overdose crisis is driven largely by exposure to illicitly-manufactured fentanyl. Preliminary observational and experimental research suggests that cannabis could potentially play a role in reducing use of prescription opioids among individuals with chronic pain. However, there is limited data on the effects of cannabis on illicit opioid consumption, particularly fentanyl, especially among individuals on opioid agonist therapy (OAT). We sought to assess the longitudinal association between cannabis use and exposure to fentanyl among people on OAT.
“Background: The ongoing opioid overdose crisis is driven largely by exposure to illicitly-manufactured fentanyl. Preliminary observational and experimental research suggests that cannabis could potentially play a role in reducing use of prescription opioids among individuals with chronic pain. However, there is limited data on the effects of cannabis on illicit opioid consumption, particularly fentanyl, especially among individuals on opioid agonist therapy (OAT). We sought to assess the longitudinal association between cannabis use and exposure to fentanyl among people on OAT.
 “Gynaecological cancers can be primary neoplasms, originating either from the reproductive tract or the products of conception, or secondary neoplasms, representative of metastatic disease. For some of these cancers, the exact causes are unknown; however, it is recognised that the precise aetiopathogeneses for most are multifactorial and include exogenous (such as diet) and endogenous factors (such as genetic predisposition), which mutually interact in a complex manner.
“Gynaecological cancers can be primary neoplasms, originating either from the reproductive tract or the products of conception, or secondary neoplasms, representative of metastatic disease. For some of these cancers, the exact causes are unknown; however, it is recognised that the precise aetiopathogeneses for most are multifactorial and include exogenous (such as diet) and endogenous factors (such as genetic predisposition), which mutually interact in a complex manner.
 “Plant-based therapies date back centuries. Cannabis sativa is one such plant that was used medicinally up until the early part of the 20th century.
“Plant-based therapies date back centuries. Cannabis sativa is one such plant that was used medicinally up until the early part of the 20th century.
 “Anticancer activity of different phenols is documented, but underlying mechanisms remain elusive. Recently, we have shown that cannabidiol kills the cells of acute lymphoblastic leukemia (ALL) by a direct interaction with mitochondria, with their consequent dysfunction.
“Anticancer activity of different phenols is documented, but underlying mechanisms remain elusive. Recently, we have shown that cannabidiol kills the cells of acute lymphoblastic leukemia (ALL) by a direct interaction with mitochondria, with their consequent dysfunction.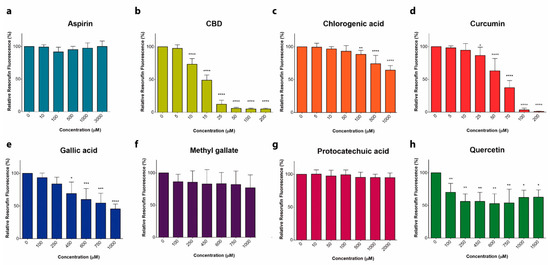
 “Cannabis sativa L. is an aromatic annual herb belonging to the family Cannabaceae and it is widely distributed worldwide. Cultivation, selling, and consumption of cannabis and cannabis related products, regardless of its use, was prohibited in Lebanon until April 22, 2020. Nevertheless, cannabis oil has been traditionally used unlawfully for many years in Lebanon to treat diseases such as arthritis, diabetes, cancer and few neurological disorders.
“Cannabis sativa L. is an aromatic annual herb belonging to the family Cannabaceae and it is widely distributed worldwide. Cultivation, selling, and consumption of cannabis and cannabis related products, regardless of its use, was prohibited in Lebanon until April 22, 2020. Nevertheless, cannabis oil has been traditionally used unlawfully for many years in Lebanon to treat diseases such as arthritis, diabetes, cancer and few neurological disorders.
 “Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder with a multifactorial etiology. Latest researches are raising the hypothesis of a link between the onset of the main behavioral symptoms of ASD and the chronic neuroinflammatory condition of the autistic brain; increasing evidence of this connection is shedding light on new possible players in the pathogenesis of ASD.
“Autism spectrum disorder (ASD) is a complex neurodevelopmental disorder with a multifactorial etiology. Latest researches are raising the hypothesis of a link between the onset of the main behavioral symptoms of ASD and the chronic neuroinflammatory condition of the autistic brain; increasing evidence of this connection is shedding light on new possible players in the pathogenesis of ASD.