 “Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.
“Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.
Recent evidence describes the use of cannabinoids in the treatment of fibromyalgia.
This study provides a systematic, thorough review of the evidence alongside a review of the seminal data regarding the pathophysiology, diagnosis, and current treatment options.
Fibromyalgia is characterized by widespread chronic pain, fatigue, and depressive episodes without an organic diagnosis, which may be prevalent in up to 10% of the population and carries a significant cost in healthcare utilization, morbidity, a reduced quality of life, and productivity. It is frequently associated with psychiatric comorbidities. The diagnosis is clinical and usually prolonged, and diagnostic criteria continue to evolve. Some therapies have been previously described, including neuropathic medications, milnacipran, and antidepressants. Despite some level of efficacy, only physical exercise has strong evidence to support it.
Cannabis has been used historically to treat different pain conditions since ancient times.
Recent advances allowed for the isolation of the active substances in cannabis and the production of cannabinoid products that are nearly devoid of psychoactive influence and provide pain relief and alleviation of other symptoms. Many of these, as well as cannabis itself, are approved for use in chronic pain conditions.
Evidence supporting cannabis in chronic pain conditions is plentiful; however, in fibromyalgia, they are mostly limited. Only a handful of randomized trials exists, and their objectivity has been questioned. However, many retrospective trials and patient surveys suggest the significant alleviation of pain, improvement in sleep, and abatement of associated symptoms.
Evidence supporting the use of cannabis in chronic pain and specifically in fibromyalgia is being gathered as the use of cannabis increases with current global trends. While the current evidence is still limited, emerging data do suggest a positive effect of cannabis in fibromyalgia.
Cannabis use is not without risks, including psychiatric, cognitive, and developmental as well as the risks of addiction. As such, clinical judgment is warranted to weigh these risks and prescribe to patients who are more likely to benefit from this treatment. Further research is required to define appropriate patient selection and treatment regimens.”
https://pubmed.ncbi.nlm.nih.gov/33004171/
https://www.sciencedirect.com/science/article/pii/S1521689620300781?via%3Dihub
 “Anxiety disorders in young people are frequently comorbid with other mental disorders and respond unsatisfactorily to first-line treatment in many cases.
“Anxiety disorders in young people are frequently comorbid with other mental disorders and respond unsatisfactorily to first-line treatment in many cases.
 “Pharmaceutically purified oral cannabidiol (CBD) has been recently approved by the US Food and Drug Administration and European Medicines Agency as treatment of seizures associated with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS), which are severe and difficult-to-treat developmental and epileptic encephalopathies with onset in early childhood.
“Pharmaceutically purified oral cannabidiol (CBD) has been recently approved by the US Food and Drug Administration and European Medicines Agency as treatment of seizures associated with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS), which are severe and difficult-to-treat developmental and epileptic encephalopathies with onset in early childhood. “Rett syndrome (RTT) is a rare neurologic disorder, characterized by severe behavioural and physiological symptoms. RTT is caused by mutations in the MECP2 gene in about 95% of cases and to date no cure is available.
“Rett syndrome (RTT) is a rare neurologic disorder, characterized by severe behavioural and physiological symptoms. RTT is caused by mutations in the MECP2 gene in about 95% of cases and to date no cure is available. “Background: Little is known about medical cannabis (MC)-related care for patients with cancer using MC.
“Background: Little is known about medical cannabis (MC)-related care for patients with cancer using MC. “∆ 9 -Tetrahydrocannabinol (∆9 -THC), the active phytocannabinoid in cannabis, is virtually an adjunct to the endogenous endocannabinoid signaling system.
“∆ 9 -Tetrahydrocannabinol (∆9 -THC), the active phytocannabinoid in cannabis, is virtually an adjunct to the endogenous endocannabinoid signaling system. “Diabetes mellitus (DM), a metabolic disorder is one of the most prevalent chronic diseases worldwide across developed as well as developing nations. Hyperglycemia is the core feature of the type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), following insulin deficiency and impaired insulin secretion or sensitivity leads insulin resistance (IR), respectively. Genetic and environmental factors attributed to the pathogenesis of DM and various therapeutic strategies are available for the prevention and treatment of T2DM.
“Diabetes mellitus (DM), a metabolic disorder is one of the most prevalent chronic diseases worldwide across developed as well as developing nations. Hyperglycemia is the core feature of the type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), following insulin deficiency and impaired insulin secretion or sensitivity leads insulin resistance (IR), respectively. Genetic and environmental factors attributed to the pathogenesis of DM and various therapeutic strategies are available for the prevention and treatment of T2DM.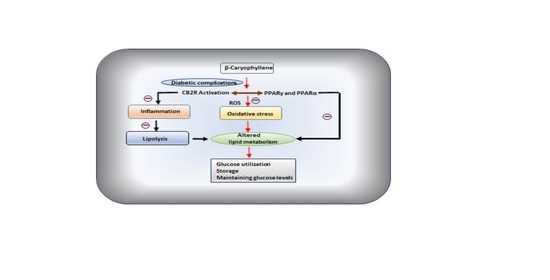
 “While activation of cannabinoid (CB2) receptors has been shown to be neuroprotective, no studies have examined whether this neuroprotection is directed at cerebral arterioles and no studies have examined whether activation of CB2 receptors can rescue cerebrovascular dysfunction during a chronic disease state such as type 1 diabetes (T1D).
“While activation of cannabinoid (CB2) receptors has been shown to be neuroprotective, no studies have examined whether this neuroprotection is directed at cerebral arterioles and no studies have examined whether activation of CB2 receptors can rescue cerebrovascular dysfunction during a chronic disease state such as type 1 diabetes (T1D). “Studies that have analyzed the association between cannabis use and acute ischemic stroke (AIS) have provided conflicting results.
“Studies that have analyzed the association between cannabis use and acute ischemic stroke (AIS) have provided conflicting results.
 “Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.
“Fibromyalgia is a complex disease process that is as prevalent as it is poorly understood. Research into the pathophysiology is ongoing, and findings will likely assist in identifying new therapeutic options to augment those in existence today that are still insufficient for the care of a large population of patients.