 “Fish oil (FO) and phytocannabinoids have received considerable attention for their intestinal anti-inflammatory effects.
“Fish oil (FO) and phytocannabinoids have received considerable attention for their intestinal anti-inflammatory effects.
We investigated whether the combination of FO with cannabigerol (CBG) and cannabidiol (CBD) or a combination of all three treatments results in a more pronounced intestinal antiinflammatory action compared to the effects achieved separately.
Colitis was induced in mice by 2,4-dinitrobenzenesulfonic acid (DNBS). CBD and CBG levels were detected and quantified by liquid chromatography coupled with time of flight mass spectrometry and ion trap mass spectrometry (LC-MS-IT-TOF). Endocannabinoids and related mediators were assessed by LC-MS. DNBS increased colon weight/colon length ratio, myeloperoxidase activity, interleukin-1β, and intestinal permeability.
CBG, but not CBD, given by oral gavage, ameliorated DNBS-induced colonic inflammation. FO pretreatment (at the inactive dose) increased the antiinflammatory action of CBG and rendered oral CBD effective while reducing endocannabinoid levels. Furthermore, the combination of FO, CBD, and a per se inactive dose of CBG resulted in intestinal anti-inflammatory effects. Finally, FO did not alter phytocannabinoid levels in the serum and in the colon.
By highlighting the apparent additivity between phytocannabinoids and FO, our preclinical data support a novel strategy of combining these substances for the potential development of a treatment of inflammatory bowel disease.”

 “Cannabidiol (CBD) is known for its vasorelaxant (including in the human pulmonary artery), anti-proliferative and anti-inflammatory properties. The aim of our study was to examine the potential preventive effect of chronic CBD administration (10 mg/kg/day for three weeks) on monocrotaline (MCT)-induced pulmonary hypertension (PH) rats.
“Cannabidiol (CBD) is known for its vasorelaxant (including in the human pulmonary artery), anti-proliferative and anti-inflammatory properties. The aim of our study was to examine the potential preventive effect of chronic CBD administration (10 mg/kg/day for three weeks) on monocrotaline (MCT)-induced pulmonary hypertension (PH) rats.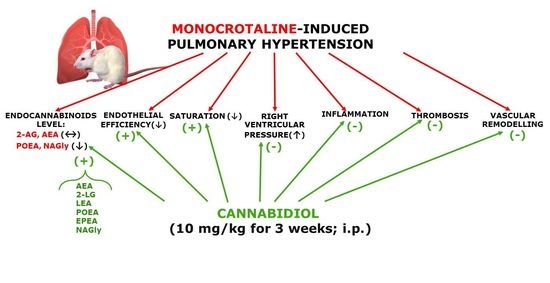
 “Pancreatic cancer (PC) is related to lifestyle risks, chronic inflammation, and germline mutations in BRCA1/2, ATM, MLH1, TP53, or CDKN2A. Surgical resection and adjuvant chemotherapy are the main therapeutic strategies but are less effective in patients with high-grade tumors.
“Pancreatic cancer (PC) is related to lifestyle risks, chronic inflammation, and germline mutations in BRCA1/2, ATM, MLH1, TP53, or CDKN2A. Surgical resection and adjuvant chemotherapy are the main therapeutic strategies but are less effective in patients with high-grade tumors.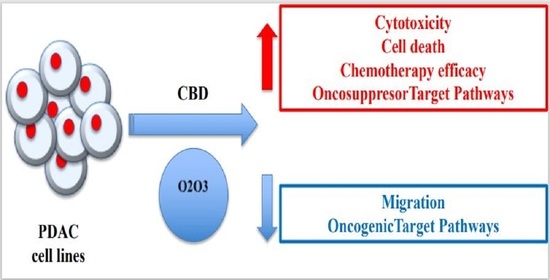
 “In recent years there has been a growing appreciation by regulatory authorities that cannabis-based medicines can play a useful role in disease therapy.
“In recent years there has been a growing appreciation by regulatory authorities that cannabis-based medicines can play a useful role in disease therapy. “Cannabidiol (CBD) is reported to produce pain relief, but the clinically relevant cellular and molecular mechanisms remain uncertain.
“Cannabidiol (CBD) is reported to produce pain relief, but the clinically relevant cellular and molecular mechanisms remain uncertain. “Cannabidiol (CBD), a natural occurring phytocannabinoid, is used extensively in consumer products ranging from foods to shampoos, topical oils and lotions.
“Cannabidiol (CBD), a natural occurring phytocannabinoid, is used extensively in consumer products ranging from foods to shampoos, topical oils and lotions. “To determine if cannabis may be used as an alternative or adjunct treatment for intermittent and chronic prescription opioid users.
“To determine if cannabis may be used as an alternative or adjunct treatment for intermittent and chronic prescription opioid users. “The prevalence of mild traumatic brain injury is highest amongst the adolescent population and can lead to complications including neuroinflammation and excitotoxicity.
“The prevalence of mild traumatic brain injury is highest amongst the adolescent population and can lead to complications including neuroinflammation and excitotoxicity.