 “Cannabis has been used for its medicinal purposes since ancient times. Its consumption leads to the activation of Cannabis receptors CB1 and CB2 that, through specific mechanisms can lead to modulation and progression of inflammation or repair. The novel findings are linked to the medical use of Cannabis in gastrointestinal (GI) system.
“Cannabis has been used for its medicinal purposes since ancient times. Its consumption leads to the activation of Cannabis receptors CB1 and CB2 that, through specific mechanisms can lead to modulation and progression of inflammation or repair. The novel findings are linked to the medical use of Cannabis in gastrointestinal (GI) system.
Purpose: The objective of the present paper is to elucidate the role of Cannabis consumption in GI system. An additional aim is to review the information on the function of Cannabis in non-alcoholic fatty liver disease (NAFLD).
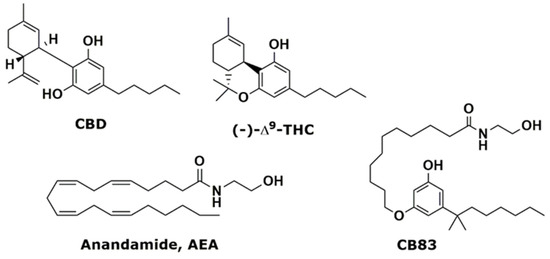
Methods and results: This review summarizes the recent findings on the role of cannabinoid receptors, their synthetic or natural ligands, as well as their metabolizing enzymes in normal GI function and its disorders, including irritable bowel syndrome (IBS), inflammatory bowel disease (IBD) and possible adverse events. The synergism or antagonism between Cannabis’ active ingredients and the “entourage” plays a role in the efficacy of various strains. Some elements of Cannabis may alter disease severity as over-activation of Cannabis receptors CB1 and CB2 can lead to changes of the commensal gut flora. The endocannabinoid system (ECS) contributes to gut homeostasis. The ability of ECS to modulate inflammatory responses demonstrates the capacity of ECS to preserve gastrointestinal (GI) function. Alterations of the ECS may predispose patients to pathologic disorders, including IBD. Clinical studies in IBD demonstrate that subjects benefit from Cannabis consumption as seen through a reduction of the IBD-inflammation, as well as through a decreased need for other medication. NAFLD is characterized by fat accumulation in the liver. The occurrence of inflammation in NAFLD leads to non-alcoholic-steatohepatitis (NASH). The use of Cannabis might reduce liver inflammation.
Conclusions: With limited evidence of efficacy and safety of Cannabis in IBD, IBS, and NAFLD, randomized controlled studies are required to examine its therapeutic efficacy.”
https://pubmed.ncbi.nlm.nih.gov/32762830/
https://journals.library.ualberta.ca/jpps/index.php/JPPS/article/view/31242

 “Purpose of review: To evaluate the impact of flavonoids and cannabinoids as anti-inflammatory and antiallergic treatments on the anterior surface of the eye.
“Purpose of review: To evaluate the impact of flavonoids and cannabinoids as anti-inflammatory and antiallergic treatments on the anterior surface of the eye. “Although several lines of evidence support the hypothesis of a dysregulation of serotoninergic neurotransmission in the pathophysiology of obsessive-compulsive disorder (OCD), there is also evidence for an involvement of other pathways such as the GABAergic, glutamatergic, and dopaminergic systems.
“Although several lines of evidence support the hypothesis of a dysregulation of serotoninergic neurotransmission in the pathophysiology of obsessive-compulsive disorder (OCD), there is also evidence for an involvement of other pathways such as the GABAergic, glutamatergic, and dopaminergic systems. “Melanoma is the fourth most common type of cancer diagnosed in Australians after breast, prostate, and colorectal cancers. While there has been substantial progress in the treatment of cancer in general, malignant melanoma, in particular, is resistant to existing medical therapies requiring an urgent need to develop effective treatments with lesser side effects.
“Melanoma is the fourth most common type of cancer diagnosed in Australians after breast, prostate, and colorectal cancers. While there has been substantial progress in the treatment of cancer in general, malignant melanoma, in particular, is resistant to existing medical therapies requiring an urgent need to develop effective treatments with lesser side effects. “The etiopathogenesis of autism spectrum disorder (ASD) remains largely unclear.
“The etiopathogenesis of autism spectrum disorder (ASD) remains largely unclear.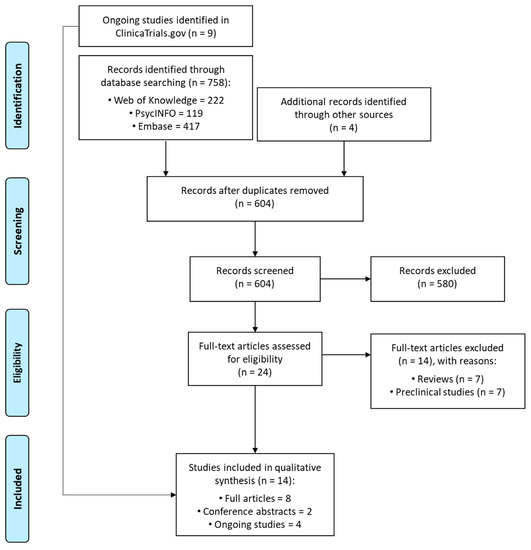
 “Posttraumatic stress disorder (PTSD) may stem from the formation of aberrant and enduring aversive memories. Some PTSD patients have recreationally used Cannabis, probably aiming at relieving their symptomatology.
“Posttraumatic stress disorder (PTSD) may stem from the formation of aberrant and enduring aversive memories. Some PTSD patients have recreationally used Cannabis, probably aiming at relieving their symptomatology.
 “Alcohol is a psychoactive substance highly used worldwide, whose harmful use might cause a broad range of mental and behavioural disorders. Underlying brain impact, the neuroinflammatory response induced by alcohol is recognised as a key contributing factor in the progression of other neuropathological processes, such as neurodegeneration. These sequels are determined by multiple factors, including age of exposure.
“Alcohol is a psychoactive substance highly used worldwide, whose harmful use might cause a broad range of mental and behavioural disorders. Underlying brain impact, the neuroinflammatory response induced by alcohol is recognised as a key contributing factor in the progression of other neuropathological processes, such as neurodegeneration. These sequels are determined by multiple factors, including age of exposure.