 “Human adipose tissue includes large quantities of mesenchymal stromal cells (atMSCs), which represent an abundant cell source for therapeutic applications in the field of regenerative medicine.
“Human adipose tissue includes large quantities of mesenchymal stromal cells (atMSCs), which represent an abundant cell source for therapeutic applications in the field of regenerative medicine.
Adipose tissue secrets various soluble factors including endocannabinoids, and atMSCs express the cannabinoid receptors CB1 and CB2. This indicates that adipose tissue possesses an endocannabinoid system (ECS). The ECS is also ascribed great significance for wound repair, e.g. by modulating inflammation. However, the exact effects of CB1/CB2 activation in human atMSCs have not been investigated, yet.
In the present study, we stimulated human atMSCs with increasing concentrations (1-30 μM) of the unspecific cannabinoid receptor ligand WIN55,212-2 and the specific CB2 agonist JWH-133, either alone or co-applied with the receptor antagonist Rimonabant (CB1) or AM 630 (CB2). We investigated the effects on metabolic activity, cell number, differentiation and cytokine release, which are important processes during tissue regeneration.
WIN decreased metabolic activity and cell number, which was reversed by Rimonabant. This suggests a CB1 dependent mechanism, whereas the number of atMSCs was increased after CB2 ligation. WIN and JWH increased the release of VEGF, TGF-β1 and HGF. Adipogenesis was enhanced by WIN, which could be reversed by blocking CB1. There was no effect on osteogenesis, and only WIN increased chondrogenic differentiation.
Our results indicate that definite activation of the cannabinoid receptors exerted different effects in atMSCs, which could be of specific value in cell-based therapy for wound regeneration.”
https://www.ncbi.nlm.nih.gov/pubmed/32006556
https://www.sciencedirect.com/science/article/abs/pii/S001448272030080X?via%3Dihub


 “Beta-caryophyllene (BCP) is a flavoring agent, whereas l-arginine (LA) is used as a food supplement.
“Beta-caryophyllene (BCP) is a flavoring agent, whereas l-arginine (LA) is used as a food supplement. “Activation of
“Activation of  “Drugs selectively targeting CB2 hold promise for treating neurodegenerative disorders, inflammation, and pain while avoiding psychotropic side effects mediated by CB1. The mechanisms underlying CB2 activation and signaling are poorly understood but critical for drug design. Here we report the cryo-EM structure of the human CB2-Gi signaling complex bound to the agonist WIN 55,212-2. The 3D structure reveals the binding mode of WIN 55,212-2 and structural determinants for distinguishing CB2 agonists from antagonists, which are supported by a pair of rationally designed agonist and antagonist. Further structural analyses with computational docking results uncover the differences between CB2 and CB1 in receptor activation, ligand recognition, and Gi coupling. These findings are expected to facilitate rational structure-based discovery of drugs targeting the
“Drugs selectively targeting CB2 hold promise for treating neurodegenerative disorders, inflammation, and pain while avoiding psychotropic side effects mediated by CB1. The mechanisms underlying CB2 activation and signaling are poorly understood but critical for drug design. Here we report the cryo-EM structure of the human CB2-Gi signaling complex bound to the agonist WIN 55,212-2. The 3D structure reveals the binding mode of WIN 55,212-2 and structural determinants for distinguishing CB2 agonists from antagonists, which are supported by a pair of rationally designed agonist and antagonist. Further structural analyses with computational docking results uncover the differences between CB2 and CB1 in receptor activation, ligand recognition, and Gi coupling. These findings are expected to facilitate rational structure-based discovery of drugs targeting the  “The legalization of
“The legalization of  “Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.
“Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.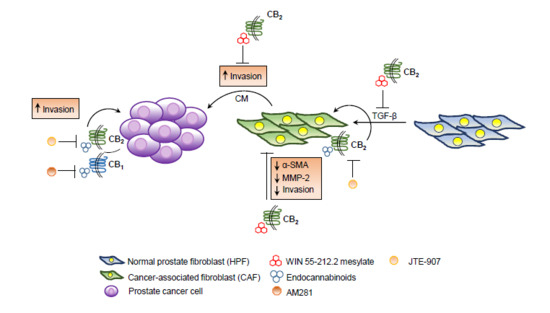
 “Recent evidence suggests that
“Recent evidence suggests that  “Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise.
“Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise.