 “The use of cannabis for skin diseases and hair regrowth is at the preliminary stage.
“The use of cannabis for skin diseases and hair regrowth is at the preliminary stage.
Legalization: Many countries have approved cannabis for medical use; however, four countries Canada, Uruguay, South Africa, and Georgia have legalized it for both medical and recreational purposes.
The endocannabinoid system: The endocannabinoid system may maintain skin homeostasis; two notable endocannabinoids include 2-Arachidonoylglycerol (2-AG) and N-arachidonoylethanolamine (AEA).
Routes of administration and pharmacokinetics: Topical cannabinoids can avoid the first-pass metabolism and reduce respiratory side effects; however, the high hydrophobicity of cannabinoids may hinder percutaneous absorption.
Skin disorders and hair growth: Human clinical studies suggest that cannabinoids may be used in eczema, acne, pruritus, and systemic sclerosis treatment. Cannabidiol (CBD) may enhance hair growth via multiple mechanisms.
Safety: Topical cannabis may cause mild side effects such as pruritus, burning, erythema, and stinging; they are relatively safer than inhalation and oral cannabis. Cannabis use may be associated with allergic symptoms and reduced immune response to live vaccination.
Cannabinoids in practice: Despite growing interest, dermatologists should be cautious prescribing cannabinoids due to insufficient clinical data on both efficacy and safety.”
https://pubmed.ncbi.nlm.nih.gov/34363728/
https://onlinelibrary.wiley.com/doi/10.1111/jocd.14352

 “Significant growth of interest in cannabis (
“Significant growth of interest in cannabis (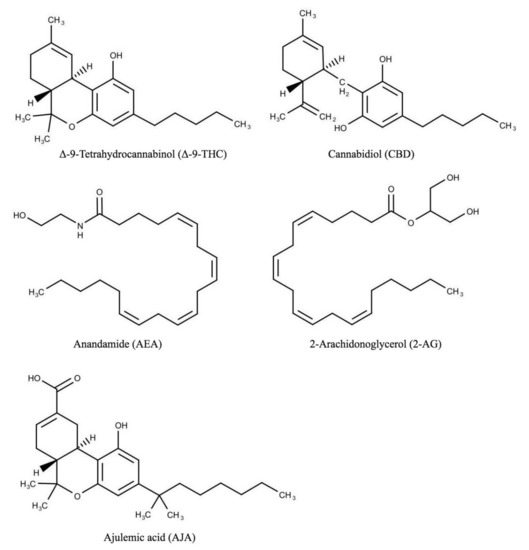

 “Background:
“Background:  “In recent decades, a lot of attention has been paid to Cannabis sativa L. due to its useful applications, including in fibers, oil, food for humans and animals, and therapeutics.
“In recent decades, a lot of attention has been paid to Cannabis sativa L. due to its useful applications, including in fibers, oil, food for humans and animals, and therapeutics.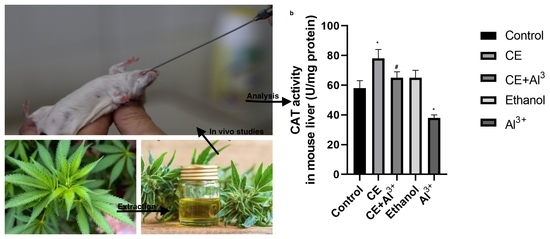
 “Background:
“Background:  “Objectives:
“Objectives:  “Cannabidiol (CBD), a phytochemical derived from
“Cannabidiol (CBD), a phytochemical derived from  “Background:
“Background: