 “Natural cannabinoids may have beneficial effects on various tissues and functions including a positive influence on the immune system and the inflammatory process.
“Natural cannabinoids may have beneficial effects on various tissues and functions including a positive influence on the immune system and the inflammatory process.
The purpose of this study was to investigate the effects of natural cannabinoids on the production of pro-inflammatory cytokines by lipopolysaccharide (LPS)-stimulated whole human blood cells.
Levels of the pro-inflammatory cytokines interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α) were measured before and after exposure of LPS-stimulated whole blood to different concentrations of Cannabidiol (CBD) or a combination of CBD and Tetrahydrocannabinol (THC) extract.
LPS stimulated the production of the pro-inflammatory cytokines. Exposure to both CBD and CBD/THC extracts significantly suppressed cytokine production in a dose-dependent manner. Exposure to cannabinoid concentrations of 50 μg/ml or 100 μg/ml resulted in a near-complete inhibition of cytokine production.
This study demonstrates that natural cannabinoids significantly suppress pro-inflammatory cytokine production in LPS-stimulated whole blood in a dose-dependent manner. The use of human whole blood, rather than isolated specific cells or tissues, may closely mimic an in vivo sepsis environment.
These findings highlight the role that natural cannabinoids may play in suppressing inflammation and call for additional studies of their use as possible novel therapeutic agents for acute and chronic inflammation.”

 “In the absence of effective antivirals and vaccination, the pandemic of COVID-19 remains the most significant challenge to our health care system in decades. There is an urgent need for definitive therapeutic intervention.
“In the absence of effective antivirals and vaccination, the pandemic of COVID-19 remains the most significant challenge to our health care system in decades. There is an urgent need for definitive therapeutic intervention. “Cannabidiol (CBD) is a non-intoxicating and generally well-tolerated constituent of cannabis which exhibits potential beneficial properties in a wide range of diseases, including cardiovascular disorders.
“Cannabidiol (CBD) is a non-intoxicating and generally well-tolerated constituent of cannabis which exhibits potential beneficial properties in a wide range of diseases, including cardiovascular disorders.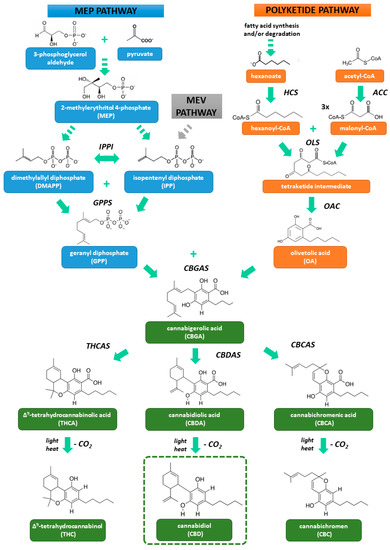
 “Mutations in SYNGAP1 are associated with developmental delay, epilepsy, and autism spectrum disorder (ASD). Epilepsy is often drug-resistant in this syndrome with frequent drop attacks.
“Mutations in SYNGAP1 are associated with developmental delay, epilepsy, and autism spectrum disorder (ASD). Epilepsy is often drug-resistant in this syndrome with frequent drop attacks. “Recent years have seen an increase in the adoption of cannabinoid medicines, which have demonstrated effectiveness for the treatment of chronic pain.
“Recent years have seen an increase in the adoption of cannabinoid medicines, which have demonstrated effectiveness for the treatment of chronic pain. “Cannabis products have been used for centuries by humans for recreational and medical purposes. Resent research, proposed the promising therapeutic potential of cannabis and related cannabinoids for a wide range of medical conditions, including psychiatric and neurological diseases.
“Cannabis products have been used for centuries by humans for recreational and medical purposes. Resent research, proposed the promising therapeutic potential of cannabis and related cannabinoids for a wide range of medical conditions, including psychiatric and neurological diseases. “Cannabis and cannabinoid-based extracts have long been utilized for their perceived therapeutic value, and support for the legalization of cannabis for medicinal purposes continues to increase worldwide.
“Cannabis and cannabinoid-based extracts have long been utilized for their perceived therapeutic value, and support for the legalization of cannabis for medicinal purposes continues to increase worldwide. “Cannabis is an annual plant with a long history of use as food, feed, fiber, oil, medicine, and narcotics. Despite realizing its true value, it has not yet found its true place. Cannabis has had a long history with many ups and downs, and now it is our turn to promote it.
“Cannabis is an annual plant with a long history of use as food, feed, fiber, oil, medicine, and narcotics. Despite realizing its true value, it has not yet found its true place. Cannabis has had a long history with many ups and downs, and now it is our turn to promote it.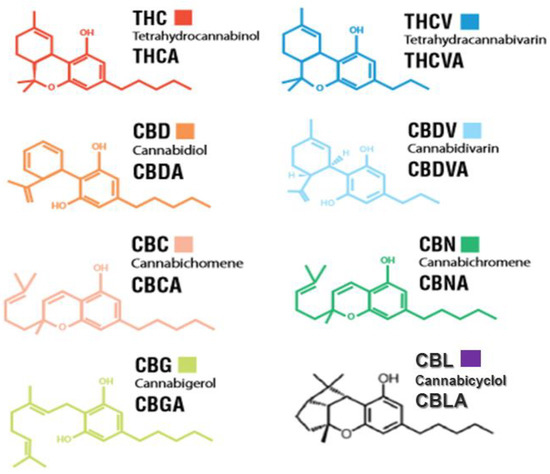
 “The immune-suppressive effects of cannabidiol (CBD) are attributed to the modulation of essential immunological signaling pathways and receptors. Mechanistic understanding of the pharmacological effects of CBD emphasizes the therapeutic potential of CBD as a novel immune modulator.
“The immune-suppressive effects of cannabidiol (CBD) are attributed to the modulation of essential immunological signaling pathways and receptors. Mechanistic understanding of the pharmacological effects of CBD emphasizes the therapeutic potential of CBD as a novel immune modulator.