 “Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.
“Endo-, phyto- and synthetic cannabinoids have been proposed as promising anti-cancer agents able to impair cancer cells’ behavior without affecting their non-transformed counterparts.
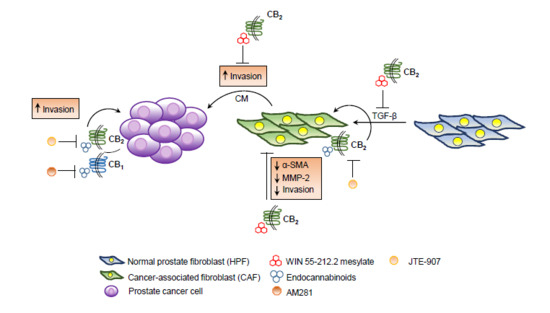
However, cancer outcome depends not only on cancer cells’ activity, but also on the stromal cells, which coevolve with cancer cells to sustain tumor progression.
Here, we show for the first time that cannabinoid treatment impairs the activation and the reactivity of cancer-associated fibroblasts (CAFs), the most represented stromal component of prostate tumor microenvironment.
Overall, our data strongly support the use of cannabinoids as anti-tumor agents in prostate cancer, since they are able to simultaneously strike both cancer and stromal cells.”
https://www.ncbi.nlm.nih.gov/pubmed/31991773
https://www.mdpi.com/1422-0067/21/3/787

 “Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise.
“Medical marijuana is becoming widely available to patients in the U.S. and with recreational marijuana now legalized in many states, patient interest is on the rise. “Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies.
“Irritable bowel syndrome (IBS) global burden is underestimated despite its high prevalence. It’s a gastrointestinal disease having obscure pathophysiology with multiple therapies yet unsatisfactory remedies. “Palliative medicine physicians are challenged by lack of guidance regarding effectiveness and dosing of cannabis products in the setting of their emerging popularity.
“Palliative medicine physicians are challenged by lack of guidance regarding effectiveness and dosing of cannabis products in the setting of their emerging popularity. “Abnormal
“Abnormal 
 “Parkinson’s disease is a neurodegenerative disorder, the motor symptoms of which are associated classically with Lewy body formation and nigrostriatal degeneration.
“Parkinson’s disease is a neurodegenerative disorder, the motor symptoms of which are associated classically with Lewy body formation and nigrostriatal degeneration.