 “Background: Canine urothelial carcinoma is the most common form of canine bladder cancer. Treatment with chemotherapy has variable response rates leading to most dogs succumbing to their disease within a year. Cannabidiol is an emerging treatment within the field of oncology. In reported in vivo studies, cannabidiol has induced apoptosis, reduced cell migration, and acted as a chemotherapy sensitizer in various human tumor types. The aim of this study was to characterize the effects of cannabidiol on canine urothelial carcinoma cell viability and apoptosis as both a single agent and in combination with chemotherapy in vitro.
“Background: Canine urothelial carcinoma is the most common form of canine bladder cancer. Treatment with chemotherapy has variable response rates leading to most dogs succumbing to their disease within a year. Cannabidiol is an emerging treatment within the field of oncology. In reported in vivo studies, cannabidiol has induced apoptosis, reduced cell migration, and acted as a chemotherapy sensitizer in various human tumor types. The aim of this study was to characterize the effects of cannabidiol on canine urothelial carcinoma cell viability and apoptosis as both a single agent and in combination with chemotherapy in vitro.
Results: Cannabidiol reduced cell viability and induced apoptosis in canine urothelial cells as determined by crystal violet viability assay and annexin V/propidium iodide flow cytometry. Furthermore, combinations of cannabidiol with mitoxantrone and vinblastine chemotherapy yielded significantly reduced cell viability and increased apoptosis compared to single agent treatment alone. The drug interactions were deemed synergistic based on combination index calculations. Conversely, the combination of cannabidiol and carboplatin did not result in decreased cell viability and increased apoptosis compared to single agent treatment. Combination index calculations suggested an antagonistic interaction between these drugs. Finally, the combination of the non-steroidal anti-inflammatory drug piroxicam with cannabidiol did not significantly affect cell viability, although, some cell lines demonstrated decreased cell viability when mitoxantrone was combined with piroxicam.
Conclusions: Cannabidiol showed promising results as a single agent or in combination with mitoxantrone and vinblastine for treatment of canine urothelial carcinoma cells. Further studies are justified to investigate whether these results are translatable in vivo.”
https://pubmed.ncbi.nlm.nih.gov/34352013/
“Cannabidiol (CBD) is a phytocannabinoid derived from the Cannabis sativa plant with well-documented analgesic, anti-inflammatory, and anxiolytic effects. This study determined that CBD treatment reduced viability and induced cell death in canine urothelial carcinoma cells in vitro. Taken together, these results suggest that CBD may be a potential treatment for use in combination with chemotherapeutic agents to improve canine UC carcinoma response rates and survival.”
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0255591

 “Nowadays cardiovascular diseases (CVDs) are the major causes for the reduction of the quality of life.
“Nowadays cardiovascular diseases (CVDs) are the major causes for the reduction of the quality of life. “Our laboratory is interested in searching for a new plant-based therapeutics to treat ovarian cancer.
“Our laboratory is interested in searching for a new plant-based therapeutics to treat ovarian cancer. “Introduction:
“Introduction: “Evidence on the use and efficacy of medical cannabis for children is limited. We examined clinical and epidemiological characteristics of medical cannabis treatment and caregiver-reported effects in children and adolescents in Switzerland.
“Evidence on the use and efficacy of medical cannabis for children is limited. We examined clinical and epidemiological characteristics of medical cannabis treatment and caregiver-reported effects in children and adolescents in Switzerland. “Ehlers-Danlos Syndromes (EDS) and related Hypermobility Spectrum Disorders (HSD) are debilitating connective tissue disorders that feature a prominent pain component for which there are limited therapeutic options for pain management.
“Ehlers-Danlos Syndromes (EDS) and related Hypermobility Spectrum Disorders (HSD) are debilitating connective tissue disorders that feature a prominent pain component for which there are limited therapeutic options for pain management.  “We present the case of an 18-year-old woman who suffered from complications of Ehlers-Danlos syndrome (EDS). Her pain was poorly controlled despite being on a myriad of analgesic medications at the time.
“We present the case of an 18-year-old woman who suffered from complications of Ehlers-Danlos syndrome (EDS). Her pain was poorly controlled despite being on a myriad of analgesic medications at the time. “In humans, various sites like cannabinoid receptors (CBR) having a binding affinity with cannabinoids are distributed on the surface of different cell types, where endocannabinoids (ECs) and derivatives of fatty acid can bind. The binding of these substance(s) triggers the activation of specific receptors required for various physiological functions, including pain sensation, memory, and appetite.
“In humans, various sites like cannabinoid receptors (CBR) having a binding affinity with cannabinoids are distributed on the surface of different cell types, where endocannabinoids (ECs) and derivatives of fatty acid can bind. The binding of these substance(s) triggers the activation of specific receptors required for various physiological functions, including pain sensation, memory, and appetite. 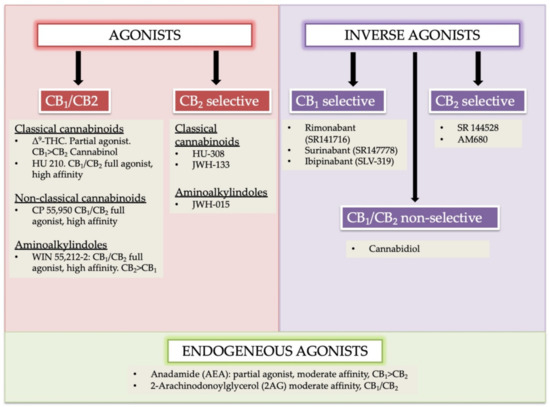
 “Chronic inflammation is considered to be a silent killer because it is the underlying cause of a wide range of clinical disorders, from cardiovascular to neurological diseases, and from cancer to obesity. In addition, there are over 80 different types of debilitating autoimmune diseases for which there are no cure. Currently, the drugs that are available to suppress chronic inflammation are either ineffective or overtly suppress the inflammation, thereby causing increased susceptibility to infections and cancer. Thus, the development of a new class of drugs that can suppress chronic inflammation is imperative.
“Chronic inflammation is considered to be a silent killer because it is the underlying cause of a wide range of clinical disorders, from cardiovascular to neurological diseases, and from cancer to obesity. In addition, there are over 80 different types of debilitating autoimmune diseases for which there are no cure. Currently, the drugs that are available to suppress chronic inflammation are either ineffective or overtly suppress the inflammation, thereby causing increased susceptibility to infections and cancer. Thus, the development of a new class of drugs that can suppress chronic inflammation is imperative. 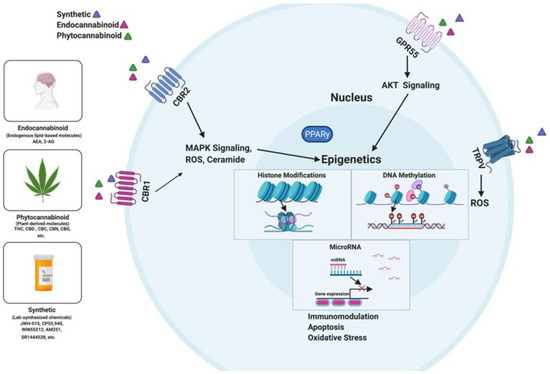
 “Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.”
“Central pain after stroke due to brainstem infarction is very rare. Treatment is difficult and specific guidelines are lacking. This is the report of a 61-year-old female patient who, after a posterolateral left medulla oblongata insult with incomplete Wallenberg syndrome, subsequently developed a burning and tingling pain in the contralateral leg and a burning and shooting pain in the ipsilateral face in trigeminal branches 1 and 2. More than 3 years of therapy with amitriptyline, gabapentin, pregabalin and various grade II and III opioids was ineffective or showed intolerable side effects. The administration of tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio improved the pain situation and quality of life quickly and permanently. The encouraging results in the present case may suggest that treatment with medical cannabis should be considered in similar cases when standard therapies are insufficient.”