“A large number of cannabinoids have been discovered that could play a role in mitigating cardiac affections. However, none of them has been as widely studied as cannabidiol (CBD), most likely because, individually, the others offer only partial effects or can activate potential harmful pathways.
In this regard, CBD has proven to be of great value as a cardioprotective agent since it is a potent antioxidant and anti-inflammatory molecule. Thus, we conducted a review to condensate the currently available knowledge on CBD as a therapy for different experimental models of cardiomyopathies and heart failure to detect the molecular pathways involved in cardiac protection.
CBD therapy can greatly limit the production of oxygen/nitrogen reactive species, thereby limiting cellular damage, protecting mitochondria, avoiding caspase activation, and regulating ionic homeostasis. Hence, it can affect myocardial contraction by restricting the activation of inflammatory pathways and cytokine secretion, lowering tissular infiltration by immune cells, and reducing the area of infarct and fibrosis formation. These effects are mediated by the activation or inhibition of different receptors and target molecules of the endocannabinoid system.
In the final part of this review, we explore the current state of CBD in clinical trials as a treatment for cardiovascular diseases and provide evidence of its potential benefits in humans.”

 “Medical cannabis and individual cannabinoids, such as tetrahydrocannabinol (THC) and cannabidiol (CBD), are receiving growing attention in both the media and the scientific literature. The Cannabis plant, however, produces over 100 different cannabinoids, and cannabigerol (CBG) serves as the precursor molecule for the most abundant phytocannabinoids.
“Medical cannabis and individual cannabinoids, such as tetrahydrocannabinol (THC) and cannabidiol (CBD), are receiving growing attention in both the media and the scientific literature. The Cannabis plant, however, produces over 100 different cannabinoids, and cannabigerol (CBG) serves as the precursor molecule for the most abundant phytocannabinoids. “Recently, cannabinoids, such as cannabidiol (CBD) and Δ9 -tetrahydrocannabinol (THC), have been the subject of intensive research and heavy scrutiny. Cannabinoids encompass a wide array of organic molecules, including those that are physiologically produced in humans, synthesized in laboratories, and extracted primarily from the Cannabis sativa plant. These organic molecules share similarities in their chemical structures as well as in their protein binding profiles. However, pronounced differences do exist in their mechanisms of action and clinical applications, which will be briefly compared and contrasted in this review. The mechanism of action of CBD and its potential applications in cancer therapy will be the major focus of this review article.”
“Recently, cannabinoids, such as cannabidiol (CBD) and Δ9 -tetrahydrocannabinol (THC), have been the subject of intensive research and heavy scrutiny. Cannabinoids encompass a wide array of organic molecules, including those that are physiologically produced in humans, synthesized in laboratories, and extracted primarily from the Cannabis sativa plant. These organic molecules share similarities in their chemical structures as well as in their protein binding profiles. However, pronounced differences do exist in their mechanisms of action and clinical applications, which will be briefly compared and contrasted in this review. The mechanism of action of CBD and its potential applications in cancer therapy will be the major focus of this review article.”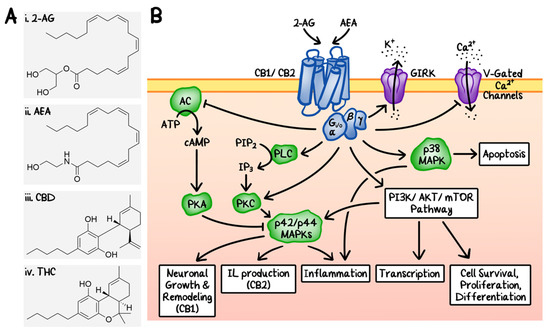
 “The aberrant accumulation of disease-specific protein aggregates accompanying cognitive decline is a pathological hallmark of age-associated neurological disorders, also termed as proteinopathies, including Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, amyotrophic lateral sclerosis and multiple sclerosis.
“The aberrant accumulation of disease-specific protein aggregates accompanying cognitive decline is a pathological hallmark of age-associated neurological disorders, also termed as proteinopathies, including Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, amyotrophic lateral sclerosis and multiple sclerosis. “Cannabidiol (CBD) is a non-psychoactive phytocannabinoid known for its beneficial effects including antioxidant and anti-inflammatory properties. Moreover, CBD is a compound with antidepressant, anxiolytic, anticonvulsant and antipsychotic effects. Thanks to all these properties, the interest of the scientific community for it has grown.
“Cannabidiol (CBD) is a non-psychoactive phytocannabinoid known for its beneficial effects including antioxidant and anti-inflammatory properties. Moreover, CBD is a compound with antidepressant, anxiolytic, anticonvulsant and antipsychotic effects. Thanks to all these properties, the interest of the scientific community for it has grown. “This article retraces the story of cannabis from the earliest contacts of humans with the plant to its subsequent global expansion, its medicinal uses, and the discovery of the endocannabinoid system in the 20th century. Cannabis was attested to around 12 000 years ago near the Altai Mountains in Central Asia, and since then, cannabis seeds have accompanied the migration of nomadic peoples. Records of the medicinal use of cannabis appear before the Common Era in China, Egypt, and Greece (Herodotus), and later in the Roman empire (Pliny the Elder, Dioscorides, Galen). In the 19th century, orientalists like Silvestre de Sacy, and Western physicians coming into contact with Muslim and Indian cultures, like O’Shaughnessy and Moreau de Tours, introduced the medicinal use of cannabis into Europe. The structure of the main psychoactive phytocannabinoid, tetrahydrocannabinol (THC), was determined in Israel by Mechoulam and Gaoni in 1964. This discovery opened the gate for many of the subsequent developments in the field of endocannabinoid system (ECS) research. The advances in the scientific knowledge of the ECS place the debate on cannabis liberalization in a new context.”
“This article retraces the story of cannabis from the earliest contacts of humans with the plant to its subsequent global expansion, its medicinal uses, and the discovery of the endocannabinoid system in the 20th century. Cannabis was attested to around 12 000 years ago near the Altai Mountains in Central Asia, and since then, cannabis seeds have accompanied the migration of nomadic peoples. Records of the medicinal use of cannabis appear before the Common Era in China, Egypt, and Greece (Herodotus), and later in the Roman empire (Pliny the Elder, Dioscorides, Galen). In the 19th century, orientalists like Silvestre de Sacy, and Western physicians coming into contact with Muslim and Indian cultures, like O’Shaughnessy and Moreau de Tours, introduced the medicinal use of cannabis into Europe. The structure of the main psychoactive phytocannabinoid, tetrahydrocannabinol (THC), was determined in Israel by Mechoulam and Gaoni in 1964. This discovery opened the gate for many of the subsequent developments in the field of endocannabinoid system (ECS) research. The advances in the scientific knowledge of the ECS place the debate on cannabis liberalization in a new context.” “Introduction and objectives: Previous studies reveal conflicting data on the effect of cannabis use in patients with cirrhosis. This research evaluates the impact of cannabis on hepatic decompensation, health care utilization, and mortality in patients with cirrhosis.
“Introduction and objectives: Previous studies reveal conflicting data on the effect of cannabis use in patients with cirrhosis. This research evaluates the impact of cannabis on hepatic decompensation, health care utilization, and mortality in patients with cirrhosis. “Background: Older adults (≥50 years) represent the fastest-growing population of people who use cannabis, potentially due to the increasing promotion of cannabis as medicine by dispensaries and cannabis websites. Given healthy aging and cannabis use are both associated with cognitive decline, it is important to establish the effects of cannabis on cognition in healthy aging.
“Background: Older adults (≥50 years) represent the fastest-growing population of people who use cannabis, potentially due to the increasing promotion of cannabis as medicine by dispensaries and cannabis websites. Given healthy aging and cannabis use are both associated with cognitive decline, it is important to establish the effects of cannabis on cognition in healthy aging. “Cannabinoids have been found to be effective in controlling seizures and the highly purified form of cannabinoid derived for Cannabis sativa . Cannabidiol (CBD) is now approved for Lennox-Gastaut syndrome (LGS) and Dravet syndrome. CBD was used in a 9-year-old boy with LGS (unknown etiology) with very good results. The electroencephalography (EEG) response was very dramatic with near normalization of EEG background and complete control of seizures. The effect of CBD on EEG with such an improvement has not been described previously. Also, this adds to evidence that early intervention in LGS with CBD might be more helpful and improve outcomes.”
“Cannabinoids have been found to be effective in controlling seizures and the highly purified form of cannabinoid derived for Cannabis sativa . Cannabidiol (CBD) is now approved for Lennox-Gastaut syndrome (LGS) and Dravet syndrome. CBD was used in a 9-year-old boy with LGS (unknown etiology) with very good results. The electroencephalography (EEG) response was very dramatic with near normalization of EEG background and complete control of seizures. The effect of CBD on EEG with such an improvement has not been described previously. Also, this adds to evidence that early intervention in LGS with CBD might be more helpful and improve outcomes.” “Chronic pelvic pain affects women across all demographics. Its management is complex and requires a multimodal approach.
“Chronic pelvic pain affects women across all demographics. Its management is complex and requires a multimodal approach.