“Cannabidiol to decrease SARS-CoV-2 associated inflammation.
Cannabidiol (CBD) is a phytocannabinoid with various clinical applications and has proven efficacy for certain medical conditions, along with a favorable safety and tolerability profile.
Cannabinoids can suppress immune activation and inflammatory cytokine production, suggesting their potential for tempering excessive inflammation.
Therefore, as SARS-CoV2 induces significant damage through pro-inflammatory cytokine storm mediated by macrophages and other immune cells and based on the fact that CBD has broad anti-inflammatory properties, CBD might represent as a potential anti-inflammatory therapeutic approach against SARS-CoV2-induced inflammation.
As CBD is already a therapeutic agent used in clinical medicine and has a favorable safety profile, the results of in vitro and animal model proof-of-concept studies would provide the necessary supporting evidence required before embarking on costly and labor-intensive clinical trials.”
https://pubmed.ncbi.nlm.nih.gov/32467020/
https://www.sciencedirect.com/science/article/pii/S1359610120301040?via%3Dihub

 “Cannabis (Cannabis sativa L.) is a complex, polymorphic plant species, which produces a vast array of bioactive metabolites, the two major chemical groups being cannabinoids and terpenoids. Nonetheless, the psychoactive cannabinoid tetrahydrocannabinol (Δ 9 -THC) and the non-psychoactive cannabidiol (CBD), are the two major cannabinoids that have monopolized the research interest.
“Cannabis (Cannabis sativa L.) is a complex, polymorphic plant species, which produces a vast array of bioactive metabolites, the two major chemical groups being cannabinoids and terpenoids. Nonetheless, the psychoactive cannabinoid tetrahydrocannabinol (Δ 9 -THC) and the non-psychoactive cannabidiol (CBD), are the two major cannabinoids that have monopolized the research interest.
 “Several neuropharmacological actions of cannabidiol (CBD) due to the modulation of the endocannabinoid system as well as direct serotonergic and gamma-aminobutyric acidergic actions have recently been identified.
“Several neuropharmacological actions of cannabidiol (CBD) due to the modulation of the endocannabinoid system as well as direct serotonergic and gamma-aminobutyric acidergic actions have recently been identified. “Four pivotal randomized placebo-controlled trials have demonstrated that adjunctive therapy with cannabidiol (CBD) improves seizure control in patients with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS).
“Four pivotal randomized placebo-controlled trials have demonstrated that adjunctive therapy with cannabidiol (CBD) improves seizure control in patients with Dravet syndrome (DS) and Lennox-Gastaut syndrome (LGS). “The market for products featuring hemp extracts is large and growing larger. However, safety concerns have been raised by medical and regulatory agencies. Post marketing surveillance of full spectrum hemp extract (FSHE) products manufactured and distributed by CV Sciences (CVSI) and traded under the brand PlusCBD™ was conducted over a 2-year period (2018-2019). The safety of these products was assessed by analyzing adverse events reports.
“The market for products featuring hemp extracts is large and growing larger. However, safety concerns have been raised by medical and regulatory agencies. Post marketing surveillance of full spectrum hemp extract (FSHE) products manufactured and distributed by CV Sciences (CVSI) and traded under the brand PlusCBD™ was conducted over a 2-year period (2018-2019). The safety of these products was assessed by analyzing adverse events reports. “Multiple sclerosis (MS) is an autoimmune demyelinating disease of the central nervous system, affecting ambulation even in people with only mild neurological signs. Patients with MS frequently experience spasticity, which contributes significantly to impair their motor functions, including ambulation, owing to muscle stiffness, spasms, and pain.
“Multiple sclerosis (MS) is an autoimmune demyelinating disease of the central nervous system, affecting ambulation even in people with only mild neurological signs. Patients with MS frequently experience spasticity, which contributes significantly to impair their motor functions, including ambulation, owing to muscle stiffness, spasms, and pain. “Cannabidiol (CBD) and cannabigerol (CBG) are Cannabis sativa terpenophenols.
“Cannabidiol (CBD) and cannabigerol (CBG) are Cannabis sativa terpenophenols.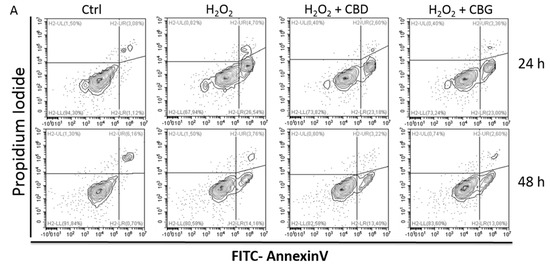
 “In this study cannabidiol (CBD) was administered orally to determine its effects and mechanisms in the experimental autoimmune encephalomyelitis (EAE) model of multiple sclerosis (MS). We hypothesized that 75 mg/kg of oral CBD given for 5 days after initiation of disease would reduce EAE severity through suppression of either the early peripheral immune or late neuroimmune response.
“In this study cannabidiol (CBD) was administered orally to determine its effects and mechanisms in the experimental autoimmune encephalomyelitis (EAE) model of multiple sclerosis (MS). We hypothesized that 75 mg/kg of oral CBD given for 5 days after initiation of disease would reduce EAE severity through suppression of either the early peripheral immune or late neuroimmune response.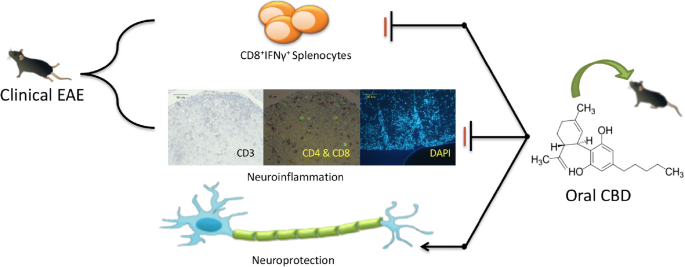
 “Cannabidiol (CBD), the major non-psychoactive constituent of Cannabis sativa L., has gained traction as a potential treatment for intractable chronic pain in many conditions. Clinical evidence suggests that CBD provides therapeutic benefit in certain forms of epilepsy and imparts analgesia in certain conditions, and improves quality of life.
“Cannabidiol (CBD), the major non-psychoactive constituent of Cannabis sativa L., has gained traction as a potential treatment for intractable chronic pain in many conditions. Clinical evidence suggests that CBD provides therapeutic benefit in certain forms of epilepsy and imparts analgesia in certain conditions, and improves quality of life.