 “The recent announcement of marijuana legalization in Canada spiked many discussions about potential health benefits of Cannabis sativa. Cannabinoids are active chemical compounds produced by cannabis, and their numerous effects on the human body are primarily exerted through interactions with cannabinoid receptor types 1 (CB1) and 2 (CB2). Cannabinoids are broadly classified as endo-, phyto-, and synthetic cannabinoids. In this review, we will describe the activity of cannabinoids on the cellular level, comprehensively summarize the activity of all groups of cannabinoids on various cancers and propose several potential mechanisms of action of cannabinoids on cancer cells.”
“The recent announcement of marijuana legalization in Canada spiked many discussions about potential health benefits of Cannabis sativa. Cannabinoids are active chemical compounds produced by cannabis, and their numerous effects on the human body are primarily exerted through interactions with cannabinoid receptor types 1 (CB1) and 2 (CB2). Cannabinoids are broadly classified as endo-, phyto-, and synthetic cannabinoids. In this review, we will describe the activity of cannabinoids on the cellular level, comprehensively summarize the activity of all groups of cannabinoids on various cancers and propose several potential mechanisms of action of cannabinoids on cancer cells.”
https://www.ncbi.nlm.nih.gov/pubmed/32249682
“Endocannabinoids and phytocannabinoids can be used for cancer therapy. Cannabis extracts have stronger anti-tumor capacity than single cannabinoids. Combination of several cannabinoids may have more potent effect on cancer.”
https://www.tandfonline.com/doi/abs/10.1080/15384101.2020.1742952?journalCode=kccy20

 “Medicinal use of
“Medicinal use of  “Since antiquity, Cannabis has provoked enormous intrigue for its potential medicinal properties as well as for its unique pharmacological effects.
“Since antiquity, Cannabis has provoked enormous intrigue for its potential medicinal properties as well as for its unique pharmacological effects. “The endocannabinoid system (ECS) comprises the canonical receptor subtypes CB1R and CB2R and endocannabinoids (anandamide, AEA and 2-arachidonoylglycerol, 2-AG), and a “non-canonical” extended signaling network consisting of: (i) other fatty acid derivatives; (ii) the defined “ionotropic cannabinoid receptors” (TRP channels); other GPCRs (GPR55, PPARα); (iii) enzymes involved in the biosynthesis and degradation of endocannabinoids (FAAH and MAGL); and (iv) protein transporters (FABP family).The ECS is currently a hot topic due to its involvement in cancer and pain.
“The endocannabinoid system (ECS) comprises the canonical receptor subtypes CB1R and CB2R and endocannabinoids (anandamide, AEA and 2-arachidonoylglycerol, 2-AG), and a “non-canonical” extended signaling network consisting of: (i) other fatty acid derivatives; (ii) the defined “ionotropic cannabinoid receptors” (TRP channels); other GPCRs (GPR55, PPARα); (iii) enzymes involved in the biosynthesis and degradation of endocannabinoids (FAAH and MAGL); and (iv) protein transporters (FABP family).The ECS is currently a hot topic due to its involvement in cancer and pain.
 “The present study investigated the effect of the lack of CB1 and CB2 receptors in mice ovarian morphology, folliculogenesis, oocyte retrieval, and oocyte maturation and evaluated the use of Δ9-tetrahydrocannabinol (THC) on oocyte in vitro maturation (IVM) by comparing classical IVM and two-step IVM by analyzing the meiotic competence of the oocytes and their evolution toward embryos.
“The present study investigated the effect of the lack of CB1 and CB2 receptors in mice ovarian morphology, folliculogenesis, oocyte retrieval, and oocyte maturation and evaluated the use of Δ9-tetrahydrocannabinol (THC) on oocyte in vitro maturation (IVM) by comparing classical IVM and two-step IVM by analyzing the meiotic competence of the oocytes and their evolution toward embryos. “The consistency, efficacy, and safety of cannabis-based medicines have been demonstrated in humans, leading to the approval of the first cannabis-based therapy to alleviate spasticity and pain associated with multiple sclerosis (MS). Indeed, the evidence supporting the therapeutic potential of
“The consistency, efficacy, and safety of cannabis-based medicines have been demonstrated in humans, leading to the approval of the first cannabis-based therapy to alleviate spasticity and pain associated with multiple sclerosis (MS). Indeed, the evidence supporting the therapeutic potential of  “For many centuries,
“For many centuries,  “Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).
“Breast cancer (BC) is the most common cancer in women worldwide. Approximately 70-80% of BCs express estrogen receptors (ER), which predict the response to endocrine therapy (ET), and are therefore hormone receptor-positive (HR+).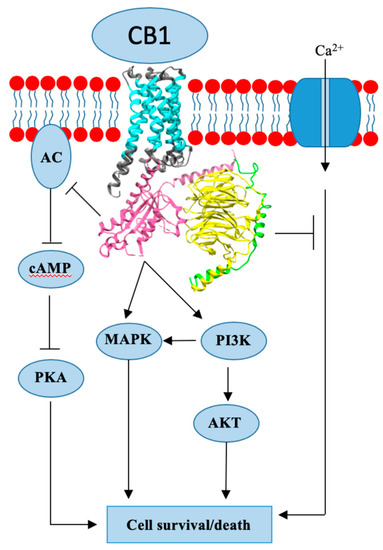
 “A growing body of literature indicates that activation of
“A growing body of literature indicates that activation of