 “Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
“Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
Like Δ9-tetrahydrocannabinol (Δ9-THC), the most well-studied cannabinoid, CBD decreased lung inflammation in a murine model of acute lung injury potentially through the inhibition of proinflammatory cytokine production by immune cells and suppressing exuberant immune responses. CBD can inhibit the production of proinflammatory cytokines like interleukin (IL)-2, IL-6, IL-1α and β, interferon gamma, inducible protein-10, monocyte chemoattractant protein-1, macrophage inflammatory protein-1α, and tumor necrosis factor-α that have been associated with SARS-CoV2 induced multi-organ pathology and mortality. In a murine model of chronic asthma, CBD reduced proinflammatory cytokine production, airway inflammation and fibrosis. Moreover, CBD can effectively inhibit the JAK-STAT pathway including the production and action of type I interferons without leading to addiction, alterations in heart rate or blood pressure and adverse effects on the gastrointestinal tract and cognition. In simian immunodeficiency virus (SIV)-infected rhesus macaques (RMs), we reported THC mediated attenuation of IFN stimulated gene expression in the intestine. Similar to CBD, chronic THC administration blocked inflammation induced fibrosis in lymph nodes of chronically SIV-infected RMs. Unlike THC, CBD has a high margin of safety and is well tolerated pharmacologically even after treatments of up to 1500 mg/day for two weeks in both animals and humans, which suggests its feasibility to reduce SARS-CoV2 induced lung inflammation/pathology and disease severity.
The many uncertainties associated with the COVID-19 pandemic such as status of the economy, employment and loss of connection can fuel depression, fear and anxiety. CBD has shown promise as an alternative therapy for the clinical management of anxiety disorders. Based on its anxiolytic and anti-depressant properties, it has been suggested that CBD could be used to improve the mental and somatic health of patients suffering from anxiety and emotional stress after recovering from Ebola disease. Like Ebola, patients recovering from COVID-19 may experience various psychological and social stressors that may be triggered by residual chronic inflammation and autoimmune reactions. Therefore, randomized clinical trials to test the efficacy of CBD on alleviating anxiety and fear associated with COVID-19 infection and its consequences on people’s physical, social and psychological well-being may be beneficial in the future. Additionally, severely ill COVID-19 patients exhibited neurological symptoms like cerebrovascular disease, headache and disturbed consciousness (Reviewed in. Brain edema, neuronal degeneration and presence of SARS-CoV2 in the cerebrospinal fluid (CSF) were confirmed at autopsy. Therefore, longitudinal CSF sampling using non-human primate (NHP) studies may help clarify whether and when SARS-CoV2 invades the brain, and if this happens, does it result in neuroinflammation and more importantly, whether cannabinoids can modulate these events.
Being a negative allosteric modulator of the cannabinoid receptor-1, CBD can counter the psychotropic effects of THC when co-administered with THC. Although Remdesivir reduced the mortality rate of seriously ill COVID-19 patients needing invasive ventilation, similar studies in rhesus macaques revealed minimal subpleural inflammatory cellular infiltrates in the lungs of clinically recovered Remdesivir treated RMs at necropsy. This suggests persistence of inflammation and may partly explain the 20–30% reduction in lung function in COVID-19 patients after recovery, which if left unresolved may lead to pulmonary fibrosis. Collectively, these findings support the investigation of cannabinoids as a plausible option to be added as an adjunct to Remdesivir or any new antivirals on SARS-CoV2 induced lung inflammation.”
https://www.ncbi.nlm.nih.gov/pubmed/32360437
https://www.sciencedirect.com/science/article/pii/S0889159120307078?via%3Dihub
“Cannabis Indica speeds up Recovery from Coronavirus” https://www.researchgate.net/publication/339746853_Cannabis_Indica_speeds_up_Recovery_from_Coronavirus

 “The intraperitoneal administration of chemotherapeutics has emerged as a potential route in ovarian cancer treatment. Nanoparticles as carriers for these agents could be interesting by increasing the retention of chemotherapeutics within the peritoneal cavity. Moreover, nanoparticles could be internalised by cancer cells and let the drug release near the biological target, which could increase the anticancer efficacy.
“The intraperitoneal administration of chemotherapeutics has emerged as a potential route in ovarian cancer treatment. Nanoparticles as carriers for these agents could be interesting by increasing the retention of chemotherapeutics within the peritoneal cavity. Moreover, nanoparticles could be internalised by cancer cells and let the drug release near the biological target, which could increase the anticancer efficacy.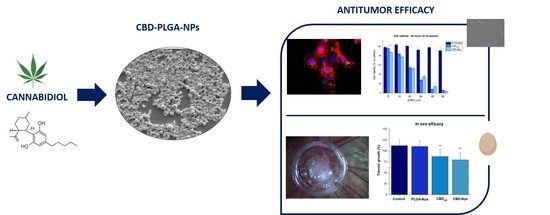

 “The therapeutic effect of the Cannabis plant largely depends on the presence and specific ratio of a spectrum of phytocannabinoids. While prescription of medicinal Cannabis for various conditions constantly grows, its consumption is mostly limited to oral or respiratory pathways, impeding its duration of action, bioavailability and efficacy. Herein, a long-acting formulation in the form of melt-printed polymeric microdepots for full-spectrum
“The therapeutic effect of the Cannabis plant largely depends on the presence and specific ratio of a spectrum of phytocannabinoids. While prescription of medicinal Cannabis for various conditions constantly grows, its consumption is mostly limited to oral or respiratory pathways, impeding its duration of action, bioavailability and efficacy. Herein, a long-acting formulation in the form of melt-printed polymeric microdepots for full-spectrum 

 “The prevalence rates of depression and anxiety are at least two times higher in diabetic patients, increasing morbidity and mortality.
“The prevalence rates of depression and anxiety are at least two times higher in diabetic patients, increasing morbidity and mortality. “Gestational methylazoxymethanol acetate (MAM) treatment produces offspring with adult phenotype relevant to schizophrenia, including positive- and negative-like symptoms, cognitive deficits, dopaminergic dysfunction, structural and functional abnormalities.
“Gestational methylazoxymethanol acetate (MAM) treatment produces offspring with adult phenotype relevant to schizophrenia, including positive- and negative-like symptoms, cognitive deficits, dopaminergic dysfunction, structural and functional abnormalities.
 “Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
“Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
 “Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
“Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.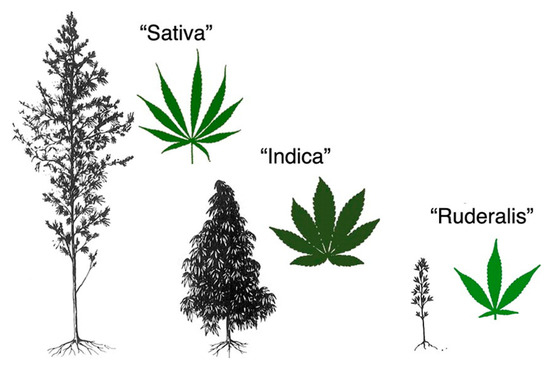
 “Parents across the United States use medical
“Parents across the United States use medical 
 “Over the last two decades, affirmative diagnoses of osteoarthritis in the United States have tripled due to increasing rates of obesity and an aging population.
“Over the last two decades, affirmative diagnoses of osteoarthritis in the United States have tripled due to increasing rates of obesity and an aging population.