“Introduction and objectives: Previous studies reveal conflicting data on the effect of cannabis use in patients with cirrhosis. This research evaluates the impact of cannabis on hepatic decompensation, health care utilization, and mortality in patients with cirrhosis.
“Introduction and objectives: Previous studies reveal conflicting data on the effect of cannabis use in patients with cirrhosis. This research evaluates the impact of cannabis on hepatic decompensation, health care utilization, and mortality in patients with cirrhosis.
Results: Cannabis use was detected in 370 (2.1%) of 17,520 cirrhotics admitted in 2011 and in 1,162 (5.3%) of 21,917 cirrhotics in 2015 (p-value <0.001). On multivariable analysis, cirrhotics utilizing cannabis after its legalization experienced a decreased rate of admissions related to hepatorenal syndrome (Odds Ratio (OR): 0.51; 95% Confidence Interval (CI): 0.34-0.78) and ascites (OR: 0.73; 95% CI: 0.63-0.84). Cirrhotics with an etiology of disease other than alcohol and hepatitis C had a higher risk of admission for hepatic encephalopathy if they utilized cannabis [OR: 1.57; 95% CI: 1.16-2.13]. Decreased length of stay (-1.15 days; 95% CI: -1.62, -0.68), total charges (-$15,852; 95% CI: -$21,009, -$10,694), and inpatient mortality (OR: 0.68; 95% CI: 0.51-0.91) were also observed in cirrhotics utilizing cannabis after legalization compared to cirrhotics not utilizing cannabis or utilizing cannabis prior to legalization.
Conclusion: Cannabis use in patients with cirrhosis resulted in mixed outcomes regarding hospital admissions with hepatic decompensation. A trend towards decreased hospital utilization and mortality was noted in cannabis users after legalization. These observations need to be confirmed with a longitudinal randomized study.”
https://pubmed.ncbi.nlm.nih.gov/33157269/
“The effectiveness of medicinal cannabis has been noted for many digestive system diseases including cirrhosis. Medicinal cannabis is associated with improved patient and hospital outcomes in cirrhotics”
https://www.sciencedirect.com/science/article/pii/S1665268120302052?via%3Dihub

 “Background: Older adults (≥50 years) represent the fastest-growing population of people who use cannabis, potentially due to the increasing promotion of cannabis as medicine by dispensaries and cannabis websites. Given healthy aging and cannabis use are both associated with cognitive decline, it is important to establish the effects of cannabis on cognition in healthy aging.
“Background: Older adults (≥50 years) represent the fastest-growing population of people who use cannabis, potentially due to the increasing promotion of cannabis as medicine by dispensaries and cannabis websites. Given healthy aging and cannabis use are both associated with cognitive decline, it is important to establish the effects of cannabis on cognition in healthy aging. “Chronic pelvic pain affects women across all demographics. Its management is complex and requires a multimodal approach.
“Chronic pelvic pain affects women across all demographics. Its management is complex and requires a multimodal approach. “(E)-β-caryophyllene (BCP) is a bicyclic sesquiterpene widely distributed in the plant kingdom, where it contributes a unique aroma to essential oils and has a pivotal role in the survival and evolution of higher plants.
“(E)-β-caryophyllene (BCP) is a bicyclic sesquiterpene widely distributed in the plant kingdom, where it contributes a unique aroma to essential oils and has a pivotal role in the survival and evolution of higher plants. “Objective: To evaluate the use of a Cannabis sativa oil in the management of patients diagnosed with primary burning mouth syndrome (BMS).
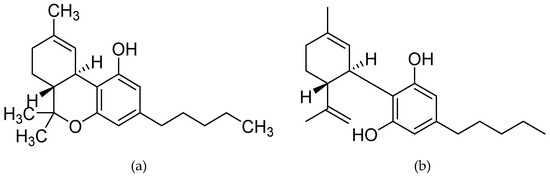
“Objective: To evaluate the use of a Cannabis sativa oil in the management of patients diagnosed with primary burning mouth syndrome (BMS). “The anti-cancer effects of cannabinoids including CBD (Cannabidiol) and THC ((-)-trans-∆9-tetrahydrocannabinol) have been reported in the case of pancreatic cancer (PC).
“The anti-cancer effects of cannabinoids including CBD (Cannabidiol) and THC ((-)-trans-∆9-tetrahydrocannabinol) have been reported in the case of pancreatic cancer (PC). “Cocaine addiction is a global health problem with no approved pharmacotherapies.
“Cocaine addiction is a global health problem with no approved pharmacotherapies. “Multiple therapeutic properties have been attributed to Cannabis sativa. However, further research is required to unveil the medicinal potential of Cannabis and the relationship between biological activity and chemical profile.
“Multiple therapeutic properties have been attributed to Cannabis sativa. However, further research is required to unveil the medicinal potential of Cannabis and the relationship between biological activity and chemical profile. “Objective: To determine the benefit of a tetrahydrocannabinol (THC)-rich cannabis oil on symptoms and quality of life of fibromyalgia patients.
“Objective: To determine the benefit of a tetrahydrocannabinol (THC)-rich cannabis oil on symptoms and quality of life of fibromyalgia patients. “Many people with MS (pwMS) use unregulated cannabis or cannabis products to treat the symptoms associated with the disease. In line with this, Sativex, a synthetic combination of cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC) has been approved to treat symptoms of spasticity.
“Many people with MS (pwMS) use unregulated cannabis or cannabis products to treat the symptoms associated with the disease. In line with this, Sativex, a synthetic combination of cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC) has been approved to treat symptoms of spasticity.