 “The therapeutic effect of the Cannabis plant largely depends on the presence and specific ratio of a spectrum of phytocannabinoids. While prescription of medicinal Cannabis for various conditions constantly grows, its consumption is mostly limited to oral or respiratory pathways, impeding its duration of action, bioavailability and efficacy. Herein, a long-acting formulation in the form of melt-printed polymeric microdepots for full-spectrum cannabidiol(CBD)-rich extract administration is described. When injected subcutaneously in mice, the microdepots facilitate sustained release of the encapsulated extract over a two-week period. The prolonged delivery results in elevated serum levels of multiple, major and minor, phytocannabinoids for over 14 days, compared to Cannabis extract injection. A direct analysis of the microdepots retrieved from the injection site gives rise to an empirical model for the release kinetics of the phytocannabinoids as a function of their physical traits. As a proof of concept, we compare the long-term efficacy of a single administration of the microdepots to a single administration of Cannabis extract in pentylenetetrazol-induced convulsions model. One week following administration, the microdepots reduce the incidence of tonic-clonic seizures by 40%, increase the survival rate by 50%, and the latency to first tonic-clonic seizures by 170%. These results suggest that a long-term full-spectrum Cannabis delivery system may provide new form of Cannabis administration and treatments.”
“The therapeutic effect of the Cannabis plant largely depends on the presence and specific ratio of a spectrum of phytocannabinoids. While prescription of medicinal Cannabis for various conditions constantly grows, its consumption is mostly limited to oral or respiratory pathways, impeding its duration of action, bioavailability and efficacy. Herein, a long-acting formulation in the form of melt-printed polymeric microdepots for full-spectrum cannabidiol(CBD)-rich extract administration is described. When injected subcutaneously in mice, the microdepots facilitate sustained release of the encapsulated extract over a two-week period. The prolonged delivery results in elevated serum levels of multiple, major and minor, phytocannabinoids for over 14 days, compared to Cannabis extract injection. A direct analysis of the microdepots retrieved from the injection site gives rise to an empirical model for the release kinetics of the phytocannabinoids as a function of their physical traits. As a proof of concept, we compare the long-term efficacy of a single administration of the microdepots to a single administration of Cannabis extract in pentylenetetrazol-induced convulsions model. One week following administration, the microdepots reduce the incidence of tonic-clonic seizures by 40%, increase the survival rate by 50%, and the latency to first tonic-clonic seizures by 170%. These results suggest that a long-term full-spectrum Cannabis delivery system may provide new form of Cannabis administration and treatments.”
Tag Archives: marijuana
Inhibitory Effect of Cannabidiol on the Activation of NLRP3 Inflammasome Is Associated with Its Modulation of the P2X7 Receptor in Human Monocytes.
 “Cannabidiol (CBD), a phytocannabinoid, has been reported to have anti-inflammatory effects associated with NLRP3 inflammasome activation, but its mechanism of anti-inflammasome action remains unclear.
“Cannabidiol (CBD), a phytocannabinoid, has been reported to have anti-inflammatory effects associated with NLRP3 inflammasome activation, but its mechanism of anti-inflammasome action remains unclear.
Herein, we report CBD’s effect on NLRP3 inflammasome activation and its modulation of P2X7, an inflammasome activation-related receptor, in human THP-1 monocytes.
Overall, the observed CBD suppressive effect on NLRP3 inflammasome activation in THP-1 monocytes was associated with decreased potassium efflux, as well as in silico prediction of P2X7 receptor binding.
CBD inhibitory effects on the NLRP3 inflammasome may contribute to the overall anti-inflammatory effects reported for this phytocannabinoid.”
https://www.ncbi.nlm.nih.gov/pubmed/32374168
https://pubs.acs.org/doi/10.1021/acs.jnatprod.0c00138

Acute and residual mood and cognitive performance of young adults following smoked cannabis.
 “To examine acute and residual mood and cognitive performance in young adult regular cannabis users following smoked cannabis.
“To examine acute and residual mood and cognitive performance in young adult regular cannabis users following smoked cannabis.
METHODS:
Ninety-one healthy young adults completed this double-blind, placebo-controlled, parallel-groups study. Participants were randomized to receive active (12.5% THC) or placebo cannabis with a 2:1 allocation ratio, and mood [Profile of Mood States (POMS)] and cognitive performance [Hopkins Verbal Learning Test – Revised (HVLT-R), Digit Symbol Substitution Test (DSST), Continuous Performance Test (CPT), grooved pegboard (GPB)] were assessed before and 1, 24, and 48 h after smoking cannabis ad libitum. High and Low THC groups were based on blood THC concentrations.
RESULTS:
One hour after smoking cannabis, compared to Placebo, in both the High and Low THC groups, there were increases in POMS Arousal and Positive Mood, and in the High THC group only, increases in Confusion, Friendliness, and Elation, and a decrease in Fatigue. Increases in Friendliness and Elation in the High THC group remained significant for 24 h. The only significant acute effect of cannabis on cognition was a decrease in the percent of words retained in the HVLT-R in the High THC group compared to Placebo (mean difference = 15.8%, 95% CI = 3.6-28.0%, p = 0.006). Unexpectedly, compared to Placebo, both the High and Low THC groups improved in DSST performance at 48 h (p ≤ 0.016).
CONCLUSIONS:
Under the present experimental conditions, in young regular cannabis users, smoking cannabis ad libitum had significant effects on mood, some of which persisted 24 h later, yet minimal effects on cognition, and no evidence of residual cognitive impairment.”
https://www.ncbi.nlm.nih.gov/pubmed/32360692
“There were few acute effects of cannabis on cognitive performance.”
https://www.sciencedirect.com/science/article/pii/S0091305719306276?via%3Dihub
The impact of naturalistic cannabis use on self-reported opioid withdrawal.
 “Four states have legalized medical cannabis for the purpose of treating opioid use disorder. It is unclear whether cannabinoids improve or exacerbate opioid withdrawal. A more thorough examination of cannabis and its impact on specific symptoms of opioid withdrawal is warranted.
“Four states have legalized medical cannabis for the purpose of treating opioid use disorder. It is unclear whether cannabinoids improve or exacerbate opioid withdrawal. A more thorough examination of cannabis and its impact on specific symptoms of opioid withdrawal is warranted.
METHOD:
Two hundred individuals recruited through Amazon Mechanical Turk with past month opioid and cannabis use and experience of opioid withdrawal completed the survey. Participants indicated which opioid withdrawal symptoms improved or worsened with cannabis use and indicated the severity of their opioid withdrawal on days with and without cannabis.
RESULTS:
62.5% (n = 125) of 200 participants had used cannabis to treat withdrawal. Participants most frequently indicated that cannabis improved: anxiety, tremors, and trouble sleeping. A minority of participants (6.0%, n = 12) indicated cannabis worsened opioid withdrawal, specifically symptoms of yawning, teary eyes, and runny nose. Across all symptoms, more participants indicated that symptoms improved with cannabis compared to those that indicated symptoms worsened with cannabis. Women reported greater relief from withdrawal with cannabis use than men.
DISCUSSION:
These results show that cannabis may improve opioid withdrawal symptoms and that the size of the effect is clinically meaningful. It is important to note that symptoms are exacerbated with cannabis in only a minority of individuals. Prospectively designed studies examining the impact of cannabis and cannabinoids on opioid withdrawal are warranted.”
https://www.ncbi.nlm.nih.gov/pubmed/32359667
“Cannabis alleviates self-reported opioid withdrawal symptoms.”
https://www.journalofsubstanceabusetreatment.com/article/S0740-5472(19)30564-1/pdf
SARS-CoV2 induced respiratory distress: Can Cannabinoids be added to anti-viral therapies to reduce lung inflammation?
 “Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
“Coronavirus disease-2019 (COVID-19), caused by Severe Acute Respiratory Syndrome coronoavirus-2 (SARS-CoV2) has emerged as a global pandemic, which was first reported in Wuhan, China. Recent reports have suggested that acute infection is associated with a cytokine superstorm, which contributes to the symptoms of fever, cough, muscle pain and in severe cases bilateral interstitial pneumonia characterized by ground glass opacity and focal chest infiltrates that can be visualized on computerized tomography scans. Currently, there are no effective antiviral drugs or vaccines against SARS-CoV2. In the recent issue of BBI, Zhang et al. thoroughly summarized the current status of potential therapeutic strategies for COVID-19. One of them, anti-IL6 receptor (Tocilizumab) antibody, resulted in clearance of lung consolidation and recovery in 90% of the 21 treated patients. Although promising, it has also produced adverse effects like pancreatitis and hypertriglyceridemia, which make it imperative to explore effective alternative anti-inflammatory strategies. Here, we intend to highlight the potential effects of cannabinoids, in particular, the non-psychotropic cannabidiol (CBD), that has shown beneficial anti-inflammatory effects in pre-clinical models of various chronic inflammatory diseases and is FDA approved for seizure reduction in children with intractable epilepsy.
Like Δ9-tetrahydrocannabinol (Δ9-THC), the most well-studied cannabinoid, CBD decreased lung inflammation in a murine model of acute lung injury potentially through the inhibition of proinflammatory cytokine production by immune cells and suppressing exuberant immune responses. CBD can inhibit the production of proinflammatory cytokines like interleukin (IL)-2, IL-6, IL-1α and β, interferon gamma, inducible protein-10, monocyte chemoattractant protein-1, macrophage inflammatory protein-1α, and tumor necrosis factor-α that have been associated with SARS-CoV2 induced multi-organ pathology and mortality. In a murine model of chronic asthma, CBD reduced proinflammatory cytokine production, airway inflammation and fibrosis. Moreover, CBD can effectively inhibit the JAK-STAT pathway including the production and action of type I interferons without leading to addiction, alterations in heart rate or blood pressure and adverse effects on the gastrointestinal tract and cognition. In simian immunodeficiency virus (SIV)-infected rhesus macaques (RMs), we reported THC mediated attenuation of IFN stimulated gene expression in the intestine. Similar to CBD, chronic THC administration blocked inflammation induced fibrosis in lymph nodes of chronically SIV-infected RMs. Unlike THC, CBD has a high margin of safety and is well tolerated pharmacologically even after treatments of up to 1500 mg/day for two weeks in both animals and humans, which suggests its feasibility to reduce SARS-CoV2 induced lung inflammation/pathology and disease severity.
The many uncertainties associated with the COVID-19 pandemic such as status of the economy, employment and loss of connection can fuel depression, fear and anxiety. CBD has shown promise as an alternative therapy for the clinical management of anxiety disorders. Based on its anxiolytic and anti-depressant properties, it has been suggested that CBD could be used to improve the mental and somatic health of patients suffering from anxiety and emotional stress after recovering from Ebola disease. Like Ebola, patients recovering from COVID-19 may experience various psychological and social stressors that may be triggered by residual chronic inflammation and autoimmune reactions. Therefore, randomized clinical trials to test the efficacy of CBD on alleviating anxiety and fear associated with COVID-19 infection and its consequences on people’s physical, social and psychological well-being may be beneficial in the future. Additionally, severely ill COVID-19 patients exhibited neurological symptoms like cerebrovascular disease, headache and disturbed consciousness (Reviewed in. Brain edema, neuronal degeneration and presence of SARS-CoV2 in the cerebrospinal fluid (CSF) were confirmed at autopsy. Therefore, longitudinal CSF sampling using non-human primate (NHP) studies may help clarify whether and when SARS-CoV2 invades the brain, and if this happens, does it result in neuroinflammation and more importantly, whether cannabinoids can modulate these events.
Being a negative allosteric modulator of the cannabinoid receptor-1, CBD can counter the psychotropic effects of THC when co-administered with THC. Although Remdesivir reduced the mortality rate of seriously ill COVID-19 patients needing invasive ventilation, similar studies in rhesus macaques revealed minimal subpleural inflammatory cellular infiltrates in the lungs of clinically recovered Remdesivir treated RMs at necropsy. This suggests persistence of inflammation and may partly explain the 20–30% reduction in lung function in COVID-19 patients after recovery, which if left unresolved may lead to pulmonary fibrosis. Collectively, these findings support the investigation of cannabinoids as a plausible option to be added as an adjunct to Remdesivir or any new antivirals on SARS-CoV2 induced lung inflammation.”
https://www.ncbi.nlm.nih.gov/pubmed/32360437
https://www.sciencedirect.com/science/article/pii/S0889159120307078?via%3Dihub
“Cannabis Indica speeds up Recovery from Coronavirus” https://www.researchgate.net/publication/339746853_Cannabis_Indica_speeds_up_Recovery_from_Coronavirus

Cannabidiol and Other Non-Psychoactive Cannabinoids for Prevention and Treatment of Gastrointestinal Disorders: Useful Nutraceuticals?
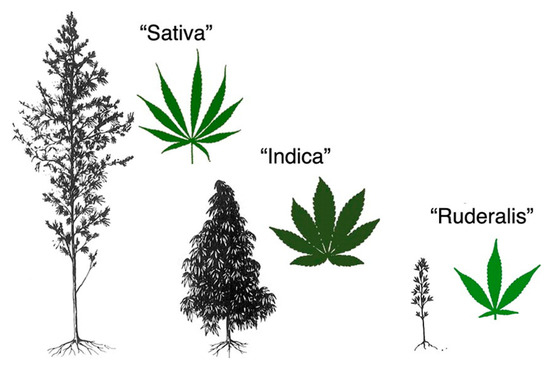
 “Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
“Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
Phytocannabinoids (terpenophenolic compounds derived from the plant), include the well-known psychoactive cannabinoid Δ9-tetrahydrocannabinol, and many non-psychoactive cannabinoids, like cannabidiol.
The endocannabinoid system (ECS) comprises of endocannabinoid ligands, enzymes for synthesis and degradation of such ligands, and receptors. This system is widely distributed in the gastrointestinal tract, where phytocannabinoids exert potent effects, particularly under pathological (i.e., inflammatory) conditions.
Herein, we will first look at the hemp plant as a possible source of new functional food ingredients and nutraceuticals that might be eventually useful to treat or even prevent gastrointestinal conditions.
Subsequently, we will briefly describe the ECS and the general pharmacology of phytocannabinoids. Finally, we will revise the available data showing that non-psychoactive phytocannabinoids, particularly cannabidiol, may be useful to treat different disorders and diseases of the gastrointestinal tract.
With the increasing interest in the development of functional foods for a healthy life, the non-psychoactive phytocannabinoids are hoped to find a place as nutraceuticals and food ingredients also for a healthy gastrointestinal tract function.”
https://www.ncbi.nlm.nih.gov/pubmed/32357565
https://www.mdpi.com/1422-0067/21/9/3067
Parents’ experiences using medical cannabis for their child.
 “Parents across the United States use medical cannabis for their children, often without professional guidance. These parents have become more expert on medical cannabis than most health professionals.
“Parents across the United States use medical cannabis for their children, often without professional guidance. These parents have become more expert on medical cannabis than most health professionals.
Using a case-study design, this study was conducted to describe the experience of parents using medical cannabis for relief of seizures in their child or dependent.
Themes revealed a complex, multifaceted experience. Many parents report benefit from medical cannabis, and are not hindered by the financial costs or uncertainties. Political and social influences have significant impact on the stigmatization and normalization of cannabis.”
https://www.ncbi.nlm.nih.gov/pubmed/32334826
“Parents across the United States are using cannabis to treat their child’s epilepsy.”
https://www.nursingoutlook.org/article/S0029-6554(19)30195-2/pdf
Cannabis and cannabinoids in cancer pain management.
 “An increasing number of patients are turning to cannabis and cannabinoids for management of their palliative and nonpalliative cancer pain and other cancer-related symptoms.
“An increasing number of patients are turning to cannabis and cannabinoids for management of their palliative and nonpalliative cancer pain and other cancer-related symptoms.
Canadians have a legal framework for access to medical cannabis, which provides a unique perspective in a setting lacking robust clinical evidence. This review seeks to delineate the role of cannabis and cannabinoids in cancer pain management and offers insight into the Canadian practice.
RECENT FINDINGS:
A cohort study using nabiximols on advanced cancer pain in patients already optimized on opioids, over 3 weeks, demonstrated improved average pain score. A large observational study of cancer patients using cannabis over 6 months demonstrated a decreased number of patients with severe pain and decreased opioid use, whereas the number of patients reporting good quality of life increased.
SUMMARY:
Good preclinical animal data and a large body of observational evidence point to the potential efficacy of cannabinoids for cancer pain management. However, there are relatively weak data pointing to clinical efficacy from clinical trial data to date. In Canada, the burgeoning cannabis industry has driven the population to embrace a medicine before clinical evidence. There remains a need for high-quality randomized controlled trials to properly assess the effectiveness and safety of medical cannabis, compared with placebo and standard treatments for cancer-related symptoms.”
https://www.ncbi.nlm.nih.gov/pubmed/32332209
https://journals.lww.com/pages/results.aspx?txtKeywords=10.1097%2fSPC.0000000000000493
Effects of THC/CBD oromucosal spray on spasticity-related symptoms in people with multiple sclerosis: results from a retrospective multicenter study.
 “The approval of 9-δ-tetrahydocannabinol (THC)+cannabidiol (CBD) oromucosal spray (Sativex®) in Italy as an add-on medication for the management of moderate to severe spasticity in multiple sclerosis (MS) has provided a new opportunity for MS patients with drug-resistant spasticity.
“The approval of 9-δ-tetrahydocannabinol (THC)+cannabidiol (CBD) oromucosal spray (Sativex®) in Italy as an add-on medication for the management of moderate to severe spasticity in multiple sclerosis (MS) has provided a new opportunity for MS patients with drug-resistant spasticity.
We aimed to investigate the improvement of MS spasticity-related symptoms in a large cohort of patients with moderate to severe spasticity in daily clinical practice.
CONCLUSION:
Our study confirmed that the therapeutic benefit of cannabinoids may extend beyond spasticity, improving spasticity-related symptoms even in non-NRS responder patients.”
https://www.ncbi.nlm.nih.gov/pubmed/32335779
https://link.springer.com/article/10.1007%2Fs10072-020-04413-6
Antimicrobial and antibiofilm activity of Cannabis sativa L. seeds extract against Staphylococcus aureus and growth effects on probiotic Lactobacillus spp.
 “The growing concern on the antibiotic resistance spreading among bacteria has stimulated the search for valuable alternatives from plant sources.
“The growing concern on the antibiotic resistance spreading among bacteria has stimulated the search for valuable alternatives from plant sources.
This study dealt with the potential use of hemp (Cannabis sativa L.) seeds extract to inhibit the growth of selected pathogenic enterobacteria and the biofilm formation by Staphylococcus aureus, representing severe risks of food-borne illnesses. Effects on probiotic bacteria were also examined. A double-staining viability/mortality assay was used to examine potential S. aureus membrane damage.
Our results highlighted a selective antimicrobial activity of C. sativa extract against pathogenic strains and no inhibitory effects on the growth of probiotic strains belonging to the Bifidobacterium and Lactobacillus genera. This selective inhibition is of outmost importance for the maintenance of healthy gut microbiota.
The double-staining assay showed that the C. sativa extract was capable of inhibiting the biofilm producer S. aureus ATCC 35556 strain; this antibacterial action was only partially linked to membrane damage. Biofilm formation was inhibited as well; inhibition occurs at lower concentration with respect to planktonic cells (0.5 mg/ml vs 1 mg/ml, respectively).
Therefore, hemp seeds extracts represent a new exploitable and valuable antimicrobial and antibiofilm agent for the food and nutraceutical industry as a possible alternative to antibiotics/antibacterial compounds.
•Cannabis sativa L. seeds showed antimicrobial and antibiofilm activity.
•C. sativa L. seeds selectively inhibit the growth of potentially pathogenic strains.
•C. sativa L. seeds did not exert antimicrobial activity against probiotic bacteria.
•C. sativa L. seeds inhibit the biofilm formation by Staphylococcus aureus.”
https://www.sciencedirect.com/science/article/pii/S0023643820301377

“Antimicrobial Activity of Cannabis sativa L.” https://www.scirp.org/journal/PaperInformation.aspx?PaperID=18123
