 “The role of the endocannabinoid system in stress-related psychiatric symptoms has been investigated in many animal and human studies.
“The role of the endocannabinoid system in stress-related psychiatric symptoms has been investigated in many animal and human studies.
Although most of these studies consistently report long-lasting effects of prolonged stress and trauma on the endocannabinoid system, the nature and direction of these changes are controversial.
We reviewed the available preclinical and clinical studies investigating the endocannabinoid system alterations long after chronic stress and trauma.
We propose that the effects of prolonged stress or trauma on the endocannabinoid system are different based on the developmental age of subjects at the time of experiencing the trauma and its repetitiveness and accumulative effects.
The current literature consistently demonstrates decreased levels of endocannabinoid ligands and receptors if the trauma occurs in childhood, whereas decreased levels of endocannabinoid ligands and increased levels of cannabinoid receptors are reported when trauma has happened in adulthood.
It is important to note that these changes are region-specific in the brain and also there are important sex differences, which are beyond the scope of this review.”
https://www.ncbi.nlm.nih.gov/pubmed/31660473
“More studies are needed to compare the effects of childhood and adulthood trauma, with or without PTSD presentations, on the eCB system. These studies would have important clinical implications, not only for individuals with trauma and PTSD who commonly have comorbid recreational cannabis use, and medical marijuana users with PTSD being one of its main indicators but also for studies investigating the potential therapeutic use of cannabinoids and eCB enhancers in PTSD treatment.”

 “WIN55,212-2 (WIN) is a synthetic agonist of
“WIN55,212-2 (WIN) is a synthetic agonist of 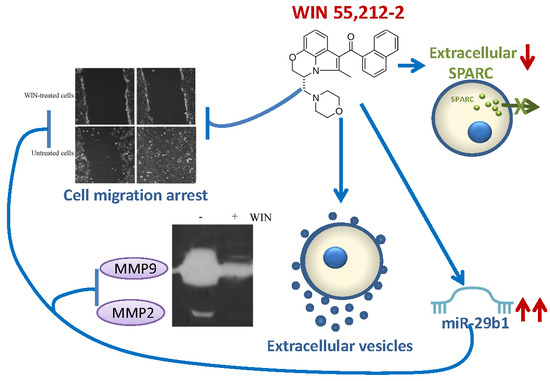
 “Medical
“Medical  “We used mouse microglial cells in culture activated by lipopolysaccharide (LPS, 10 ng/ml) to study the anti-inflammatory potential of
“We used mouse microglial cells in culture activated by lipopolysaccharide (LPS, 10 ng/ml) to study the anti-inflammatory potential of  “Excessive daytime sleepiness and cataplexy are among the symptoms of narcolepsy, a sleep disorder caused by the loss of hypocretin/orexin (HCRT/OX) neurons placed into the hypothalamus (LH). Several treatments for managing narcolepsy include diverse drugs to induce alertness, such as antidepressants, amphetamine, or modafinil, etc.
“Excessive daytime sleepiness and cataplexy are among the symptoms of narcolepsy, a sleep disorder caused by the loss of hypocretin/orexin (HCRT/OX) neurons placed into the hypothalamus (LH). Several treatments for managing narcolepsy include diverse drugs to induce alertness, such as antidepressants, amphetamine, or modafinil, etc. “Parkinson’s disease (PD) and L-DOPA-induced dyskinesia (LID) are motor disorders with significant impact on the patient’s quality of life. Unfortunately, pharmacological treatments that improve these disorders without causing severe side effects are not yet available. Delay in initiating L-DOPA is no longer recommended as LID development is a function of disease duration rather than cumulative L-DOPA exposure.
“Parkinson’s disease (PD) and L-DOPA-induced dyskinesia (LID) are motor disorders with significant impact on the patient’s quality of life. Unfortunately, pharmacological treatments that improve these disorders without causing severe side effects are not yet available. Delay in initiating L-DOPA is no longer recommended as LID development is a function of disease duration rather than cumulative L-DOPA exposure. “The high frequency and painful profile of inflammatory oral lesions and the lack of an effective drug protocol for their management stimulate the search for pharmacological alternatives for the treatment of these conditions.
“The high frequency and painful profile of inflammatory oral lesions and the lack of an effective drug protocol for their management stimulate the search for pharmacological alternatives for the treatment of these conditions.  “Modulation of
“Modulation of  “Cannabis sativa (cannabis) is one of the oldest plants cultivated by men. Cannabidiol (CBD) is the major non-psychomimetic compound derived from cannabis. It has been proposed to have a therapeutic potential over a wide range of neuropsychiatric disorders.
“Cannabis sativa (cannabis) is one of the oldest plants cultivated by men. Cannabidiol (CBD) is the major non-psychomimetic compound derived from cannabis. It has been proposed to have a therapeutic potential over a wide range of neuropsychiatric disorders.