“Breast cancer is the leading cause of cancer-related death in women worldwide. In the last years, cannabinoids have gained attention in the clinical setting and clinical trials with cannabinoid-based preparations are underway. However, contradictory anti-tumour properties have also been reported. Thus, the elucidation of the molecular mechanisms behind their anti-tumour efficacy is crucial to better understand its therapeutic potential.
“Breast cancer is the leading cause of cancer-related death in women worldwide. In the last years, cannabinoids have gained attention in the clinical setting and clinical trials with cannabinoid-based preparations are underway. However, contradictory anti-tumour properties have also been reported. Thus, the elucidation of the molecular mechanisms behind their anti-tumour efficacy is crucial to better understand its therapeutic potential.
Considering this, our work aims to clarify the molecular mechanisms underlying the anti-cancer properties of the endocannabinoid anandamide (AEA) and of the phytocannabinoids, cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC), in estrogen receptor-positive (ER+) breast cancer cells that overexpress aromatase (MCF-7aro). Their in vitro effects on cell proliferation, cell death and activity/expression of aromatase, ERα, ERβ and AR were investigated.
Our results demonstrated that cannabinoids disrupted MCF-7aro cell cycle progression. Unlike AEA and THC that induced apoptosis, CBD triggered autophagy to promote apoptotic cell death. Interestingly, all cannabinoids reduced aromatase and ERα expression levels in cells. On the other hand, AEA and CBD not only exhibited high anti-aromatase activity but also induced up-regulation of ERβ. Therefore, all cannabinoids, albeit by different actions, target aromatase and ERs, impairing, in that way, the growth of ER+ breast cancer cells, which is dependent on estrogen signalling.
As aromatase and ERs are key targets for ER+ breast cancer treatment, cannabinoids can be considered as potential and attractive therapeutic compounds for this type of cancer, being CBD the most promising one. Thus, from an in vitro perspective, this work may contribute to the growing mass of evidence of cannabinoids and cannabinoids-based medicines as potential anti-cancer drugs.”
https://pubmed.ncbi.nlm.nih.gov/33722705/
“AEA and THC induce apoptosis in ER+ breast cancer cells, while CBD trigger autophagy to promote apoptosis. AEA, THC and CBD impair growth of ER+ breast cancer cells, by disrupting cycle progression. AEA, THC and CBD affect aromatase and ERα expression levels in ER+ breast cancer cells. AEA and CBD strongly inhibited aromatase activity and up-regulated ERβ levels. Cannabinoids are considered potential therapeutic compounds for ER+ breast cancer, being CBD the most promising one.”
https://www.sciencedirect.com/science/article/abs/pii/S0960076021000698?via%3Dihub

 “The rapid spread of COVID-19 underscores the need for new treatments.
“The rapid spread of COVID-19 underscores the need for new treatments. “The main aspects of severe COVID-19 disease pathogenesis include hyper-induction of proinflammatory cytokines, also known as ‘cytokine storm’, that precedes acute respiratory distress syndrome (ARDS) and often leads to death. COVID-19 patients often suffer from lung fibrosis, a serious and untreatable condition. There remains no effective treatment for these complications.
“The main aspects of severe COVID-19 disease pathogenesis include hyper-induction of proinflammatory cytokines, also known as ‘cytokine storm’, that precedes acute respiratory distress syndrome (ARDS) and often leads to death. COVID-19 patients often suffer from lung fibrosis, a serious and untreatable condition. There remains no effective treatment for these complications. “Cannabidiol (CBD) has been shown to slow cancer cell growth and is toxic to human glioblastoma cell lines. Thus, CBD could be an effective therapeutic for glioblastoma.
“Cannabidiol (CBD) has been shown to slow cancer cell growth and is toxic to human glioblastoma cell lines. Thus, CBD could be an effective therapeutic for glioblastoma.
 “Glioblastomas (GBMs) are aggressive brain tumors with frequent genetic alterations in TP53 and PTEN tumor suppressor genes rendering resistance to standard chemotherapeutics. Cannabinoid type 1 and 2 (CB1/CB2) receptor expression in GBMs and antitumor activity of cannabinoids in glioma cells and animal models, raised promises for a targeted treatment of these tumors. The susceptibility of human glioma cells to CB2-agonists and their mechanism of action are not fully elucidated. We determined CB1 and CB2 expression in 14 low-grade and 21 high-grade tumor biopsies, GBM-derived primary cultures and established cell lines. The non-selective CB receptor agonist WIN55,212-2 (but not its inactive enantiomer) or the CB2-selective agonist JWH133 induced apoptosis in patient-derived glioma cultures and five established glioma cell lines despite p53 and/or PTEN deficiency. Growth inhibitory efficacy of cannabinoids correlated with CB1/CB2 expression (EC50 WIN55,212-2: 7.36-15.70 µM, JWH133: 12.15-143.20 µM). Treatment with WIN55,212-2 or JWH133 led to activation of the apoptotic mitochondrial pathway and DNA fragmentation. Synthetic cannabinoid action was associated with the induction of autophagy and knockdown of autophagy genes augmented cannabinoid-induced apoptotic cell death. The high susceptibility of human glioblastoma cells to synthetic cannabinoids, despite genetic defects contributing to apoptosis resistance, makes cannabinoids promising anti-glioma therapeutics.”
“Glioblastomas (GBMs) are aggressive brain tumors with frequent genetic alterations in TP53 and PTEN tumor suppressor genes rendering resistance to standard chemotherapeutics. Cannabinoid type 1 and 2 (CB1/CB2) receptor expression in GBMs and antitumor activity of cannabinoids in glioma cells and animal models, raised promises for a targeted treatment of these tumors. The susceptibility of human glioma cells to CB2-agonists and their mechanism of action are not fully elucidated. We determined CB1 and CB2 expression in 14 low-grade and 21 high-grade tumor biopsies, GBM-derived primary cultures and established cell lines. The non-selective CB receptor agonist WIN55,212-2 (but not its inactive enantiomer) or the CB2-selective agonist JWH133 induced apoptosis in patient-derived glioma cultures and five established glioma cell lines despite p53 and/or PTEN deficiency. Growth inhibitory efficacy of cannabinoids correlated with CB1/CB2 expression (EC50 WIN55,212-2: 7.36-15.70 µM, JWH133: 12.15-143.20 µM). Treatment with WIN55,212-2 or JWH133 led to activation of the apoptotic mitochondrial pathway and DNA fragmentation. Synthetic cannabinoid action was associated with the induction of autophagy and knockdown of autophagy genes augmented cannabinoid-induced apoptotic cell death. The high susceptibility of human glioblastoma cells to synthetic cannabinoids, despite genetic defects contributing to apoptosis resistance, makes cannabinoids promising anti-glioma therapeutics.”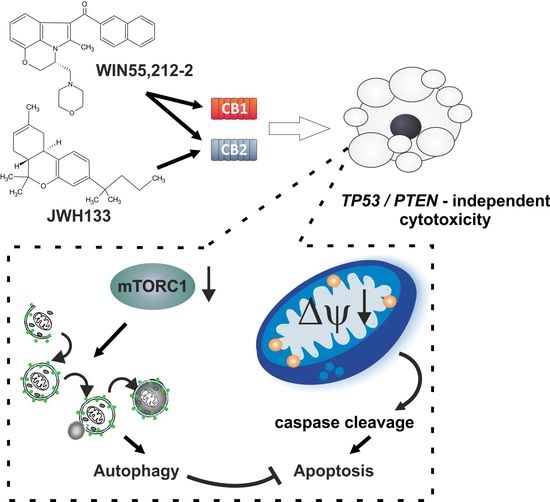
 “Glioblastoma is the most aggressive cancer among primary brain tumours. As with other cancers, the incidence of glioblastoma is increasing; despite modern therapies, the overall mean survival of patients post-diagnosis averages around 16 months, a figure that has not changed in many years. Cannabigerol (CBG) has only recently been reported to prevent the progression of certain carcinomas and has not yet been studied in glioblastoma. Here, we have compared the cytotoxic, apoptotic, and anti-invasive effects of the purified natural cannabinoid CBG together with CBD and THC on established differentiated glioblastoma tumour cells and glioblastoma stem cells. CBG and THC reduced the viability of both types of cells to a similar extent, whereas combining CBD with CBG was more efficient than with THC. CBD and CBG, both alone and in combination, induced caspase-dependent cell apoptosis, and there was no additive THC effect. Of note, CBG inhibited glioblastoma invasion in a similar manner to CBD and the chemotherapeutic temozolomide. We have demonstrated that THC has little added value in combined-cannabinoid glioblastoma treatment, suggesting that this psychotropic cannabinoid should be replaced with CBG in future clinical studies of glioblastoma therapy.”
“Glioblastoma is the most aggressive cancer among primary brain tumours. As with other cancers, the incidence of glioblastoma is increasing; despite modern therapies, the overall mean survival of patients post-diagnosis averages around 16 months, a figure that has not changed in many years. Cannabigerol (CBG) has only recently been reported to prevent the progression of certain carcinomas and has not yet been studied in glioblastoma. Here, we have compared the cytotoxic, apoptotic, and anti-invasive effects of the purified natural cannabinoid CBG together with CBD and THC on established differentiated glioblastoma tumour cells and glioblastoma stem cells. CBG and THC reduced the viability of both types of cells to a similar extent, whereas combining CBD with CBG was more efficient than with THC. CBD and CBG, both alone and in combination, induced caspase-dependent cell apoptosis, and there was no additive THC effect. Of note, CBG inhibited glioblastoma invasion in a similar manner to CBD and the chemotherapeutic temozolomide. We have demonstrated that THC has little added value in combined-cannabinoid glioblastoma treatment, suggesting that this psychotropic cannabinoid should be replaced with CBG in future clinical studies of glioblastoma therapy.” “Background: Breast Cancer (BC), a common death-causing disease and the deadliest cancer next to lung cancer, is characterized by an abnormal growth of cells in the tissues of the breast. BC chemotherapy is marked by targeting the activities of some receptors such as Estrogen Receptor alpha (ER-α). At present, one of the most commonly used and approved marketed therapeutic drug for BC is tamoxifen. Despite the short term success of tamoxifen usage, its long time treatment has been associated with significant side effects. Therefore, there is a pressing need for the development of novel anti-estrogens for the prevention and treatment of BC.
“Background: Breast Cancer (BC), a common death-causing disease and the deadliest cancer next to lung cancer, is characterized by an abnormal growth of cells in the tissues of the breast. BC chemotherapy is marked by targeting the activities of some receptors such as Estrogen Receptor alpha (ER-α). At present, one of the most commonly used and approved marketed therapeutic drug for BC is tamoxifen. Despite the short term success of tamoxifen usage, its long time treatment has been associated with significant side effects. Therefore, there is a pressing need for the development of novel anti-estrogens for the prevention and treatment of BC. “Considering the advantages of using medicinal herbs as supplementary treatments to sensitize conventional anti-cancer drugs, studying functional mechanisms and regulatory effects of Echinacea purpurea (as a non-cannabinoid plant)
“Considering the advantages of using medicinal herbs as supplementary treatments to sensitize conventional anti-cancer drugs, studying functional mechanisms and regulatory effects of Echinacea purpurea (as a non-cannabinoid plant) 


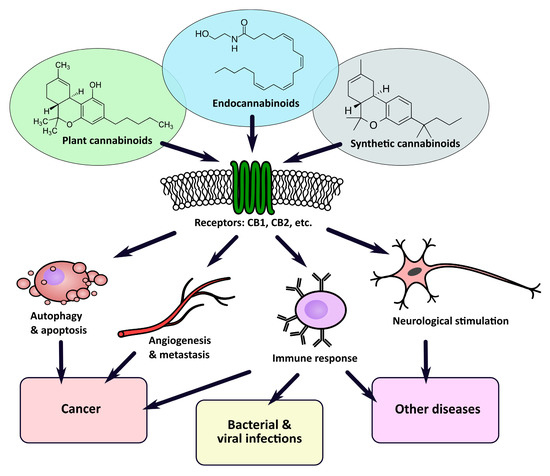
 “Derivatives of the plant Cannabis sativa have been used for centuries for both medical and recreational purposes, as well as industrial. The first proof of its medicinal use comes from ancient China, although there is evidence of its earlier utilization in Europe and Asia. In the 19th century, European practitioners started to employ cannabis extracts to treat tetanus, convulsions, and mental diseases and, in 1851, cannabis made its appearance in the Pharmacopoeia of the United States as an analgesic, hypnotic and anticonvulsant. It was only in 1937 that the Marijuana Tax Act prohibited the use of this drug in the USA. The general term Cannabis is commonly used by the scientific and scholar community to indicate derivatives of the plant Cannabis sativa. The word cannabinoid is a term describing chemical compounds that are either derivate of Cannabis (phytocannabinoids) or artificial analogues (synthetic) or are produced endogenously by the body (endocannabinoids). A more casual term “marijuana” or “weed”, a compound derived from dried Cannabis flower tops and leaves, has progressively superseded the term cannabis when referred to its recreational use. The 2018 World health organisation (WHO) data suggest that nearly 2.5% of the global population (147 million) uses marijuana and some countries, such as Canada and Uruguay, have already legalised it. Due to its controversial history, the medicinal use of cannabinoids has always been a centre of debate. The isolation and characterisation of Δ9 tetrahydrocannabinol (THC), the major psychoactive component of cannabis and the detection of two human cannabinoid receptor (CBRs) molecules renewed interest in the medical use of cannabinoids, boosting research and commercial heed in this sector. Some cannabinoid-based drugs have been approved as medications, mainly as antiemetic, antianorexic, anti-seizure remedies and in cancer and multiple sclerosis patients’ palliative care. Nevertheless, due to the stigma commonly associated with these compounds, cannabinoids’ potential in the treatment of conditions such as cancer is still largely unknown and therefore underestimated.”
“Derivatives of the plant Cannabis sativa have been used for centuries for both medical and recreational purposes, as well as industrial. The first proof of its medicinal use comes from ancient China, although there is evidence of its earlier utilization in Europe and Asia. In the 19th century, European practitioners started to employ cannabis extracts to treat tetanus, convulsions, and mental diseases and, in 1851, cannabis made its appearance in the Pharmacopoeia of the United States as an analgesic, hypnotic and anticonvulsant. It was only in 1937 that the Marijuana Tax Act prohibited the use of this drug in the USA. The general term Cannabis is commonly used by the scientific and scholar community to indicate derivatives of the plant Cannabis sativa. The word cannabinoid is a term describing chemical compounds that are either derivate of Cannabis (phytocannabinoids) or artificial analogues (synthetic) or are produced endogenously by the body (endocannabinoids). A more casual term “marijuana” or “weed”, a compound derived from dried Cannabis flower tops and leaves, has progressively superseded the term cannabis when referred to its recreational use. The 2018 World health organisation (WHO) data suggest that nearly 2.5% of the global population (147 million) uses marijuana and some countries, such as Canada and Uruguay, have already legalised it. Due to its controversial history, the medicinal use of cannabinoids has always been a centre of debate. The isolation and characterisation of Δ9 tetrahydrocannabinol (THC), the major psychoactive component of cannabis and the detection of two human cannabinoid receptor (CBRs) molecules renewed interest in the medical use of cannabinoids, boosting research and commercial heed in this sector. Some cannabinoid-based drugs have been approved as medications, mainly as antiemetic, antianorexic, anti-seizure remedies and in cancer and multiple sclerosis patients’ palliative care. Nevertheless, due to the stigma commonly associated with these compounds, cannabinoids’ potential in the treatment of conditions such as cancer is still largely unknown and therefore underestimated.” “Recently, there has been a growing interest in the medical applications of Cannabis plants. They owe their unique properties to a group of secondary metabolites known as phytocannabinoids, which are specific for this genus. Phytocannabinoids, and cannabinoids generally, can interact with cannabinoid receptors being part of the endocannabinoid system present in animals. Over the years a growing body of scientific evidence has been gathered, suggesting that these compounds have therapeutic potential.
“Recently, there has been a growing interest in the medical applications of Cannabis plants. They owe their unique properties to a group of secondary metabolites known as phytocannabinoids, which are specific for this genus. Phytocannabinoids, and cannabinoids generally, can interact with cannabinoid receptors being part of the endocannabinoid system present in animals. Over the years a growing body of scientific evidence has been gathered, suggesting that these compounds have therapeutic potential.