 “Plant-based therapies date back centuries. Cannabis sativa is one such plant that was used medicinally up until the early part of the 20th century.
“Plant-based therapies date back centuries. Cannabis sativa is one such plant that was used medicinally up until the early part of the 20th century.
Although rich in diverse and interesting phytochemicals, cannabis was largely ignored by the modern scientific community due to its designation as a schedule 1 narcotic and restrictions on access for research purposes. There was renewed interest in the early 1990s when the endocannabinoid system (ECS) was discovered, a complex network of signaling pathways responsible for physiological homeostasis. Two key components of the ECS, cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2), were identified as the molecular targets of the phytocannabinoid Δ9-tetrahydrocannabinol (Δ9-THC).
Restrictions on access to cannabis have eased worldwide, leading to a resurgence in interest in the therapeutic potential of cannabis. Much of the focus has been on the two major constituents, Δ9-THC and cannabidiol (CBD). Cannabis contains over 140 phytocannabinoids, although only a handful have been tested for pharmacological activity. Many of these minor cannabinoids potently modulate receptors, ionotropic channels, and enzymes associated with the ECS and show therapeutic potential individually or synergistically with other phytocannabinoids.
The following review will focus on the pharmacological developments of the next generation of phytocannabinoid therapeutics.”
https://pubmed.ncbi.nlm.nih.gov/33356248/
https://pubs.acs.org/doi/10.1021/acs.jnatprod.0c00965


 “Melanoma causes the highest number of skin cancer-related deaths worldwide. New treatment methods are essential for the management of this life-threatening disease.
“Melanoma causes the highest number of skin cancer-related deaths worldwide. New treatment methods are essential for the management of this life-threatening disease. “Cannabis is increasingly being used for medicinal purposes but remains outside Western medical practice. Data on perioperative use and outcomes are scarce. Few surgeons receive training regarding legal endorsement, reported medicinal benefits, and potential risks, making it difficult to advise patients. Guidelines and additional research are needed.
“Cannabis is increasingly being used for medicinal purposes but remains outside Western medical practice. Data on perioperative use and outcomes are scarce. Few surgeons receive training regarding legal endorsement, reported medicinal benefits, and potential risks, making it difficult to advise patients. Guidelines and additional research are needed. “UV radiation is a well-established environmental risk factor known to cause oxidative stress and disrupt the metabolism of keratinocyte phospholipids. Cannabidiol (CBD) is a phytocannabinoid with anti-inflammatory and antioxidant effects.
“UV radiation is a well-established environmental risk factor known to cause oxidative stress and disrupt the metabolism of keratinocyte phospholipids. Cannabidiol (CBD) is a phytocannabinoid with anti-inflammatory and antioxidant effects.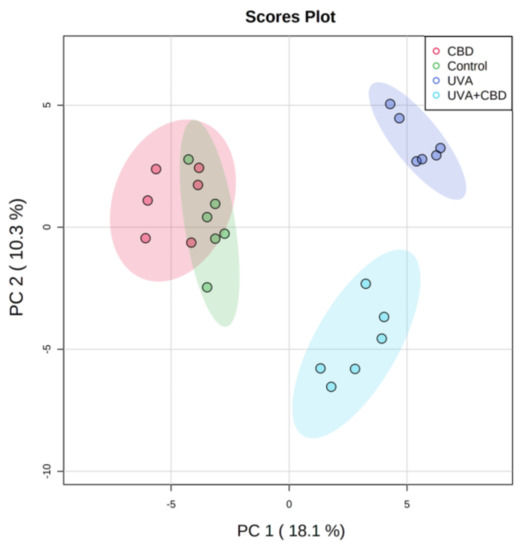
 “There is not a single pharmacological agent with demonstrated therapeutic efficacy for traumatic brain injury (TBI). With recent legalization efforts and the growing popularity of medical cannabis, patients with TBI will inevitably consider medical cannabis as a treatment option.
“There is not a single pharmacological agent with demonstrated therapeutic efficacy for traumatic brain injury (TBI). With recent legalization efforts and the growing popularity of medical cannabis, patients with TBI will inevitably consider medical cannabis as a treatment option. “Alzheimer’s disease (AD) is characterized by structural damage, death, and functional disruption of cholinergic neurons (ChNs) as a result of intracellular amyloid-β (Aβ) aggregation, extracellular neuritic plaques, and hyperphosphorylation of protein tau (p-Tau) overtime.
“Alzheimer’s disease (AD) is characterized by structural damage, death, and functional disruption of cholinergic neurons (ChNs) as a result of intracellular amyloid-β (Aβ) aggregation, extracellular neuritic plaques, and hyperphosphorylation of protein tau (p-Tau) overtime. “Chronic pelvic pain (CPP) affects up to 15% of women in the United States. The endocannabinoid system is a potential pharmacological target for pelvic pain as cannabinoid receptors are highly expressed in the uterus and other nonreproductive tissues.
“Chronic pelvic pain (CPP) affects up to 15% of women in the United States. The endocannabinoid system is a potential pharmacological target for pelvic pain as cannabinoid receptors are highly expressed in the uterus and other nonreproductive tissues. “Cannabis has long been used for healing and recreation in several regions of the world. Over 400 bioactive constituents, including more than 100 phytocannabinoids, have been isolated from this plant. The non-psychoactive cannabidiol (CBD) and the psychoactive Δ9-tetrahydrocannabinol (Δ9-THC) are the major and widely studied constituents from this plant.
“Cannabis has long been used for healing and recreation in several regions of the world. Over 400 bioactive constituents, including more than 100 phytocannabinoids, have been isolated from this plant. The non-psychoactive cannabidiol (CBD) and the psychoactive Δ9-tetrahydrocannabinol (Δ9-THC) are the major and widely studied constituents from this plant. “Research within a gynecologic oncology population has lagged behind the uptake in use of medical cannabis for symptom control. This study seeks to evaluate patient experience with prescribed medical cannabis obtained through licensed dispensaries in women with gynecologic malignancies.
“Research within a gynecologic oncology population has lagged behind the uptake in use of medical cannabis for symptom control. This study seeks to evaluate patient experience with prescribed medical cannabis obtained through licensed dispensaries in women with gynecologic malignancies.