 “The potential therapeutic use of some Cannabis sativa plant compounds has been attracting great interest, especially for managing neuropsychiatric disorders due to the relative lack of efficacy of the current treatments.
“The potential therapeutic use of some Cannabis sativa plant compounds has been attracting great interest, especially for managing neuropsychiatric disorders due to the relative lack of efficacy of the current treatments.
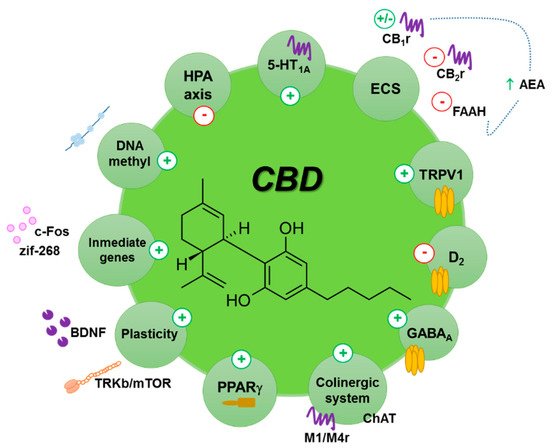
Numerous studies have been carried out using the main phytocannabinoids, tetrahydrocannabinol (THC) and cannabidiol (CBD). CBD displays an interesting pharmacological profile without the potential for becoming a drug of abuse, unlike THC.
In this review, we focused on the anxiolytic, antidepressant, and antipsychotic effects of CBD found in animal and human studies. In rodents, results suggest that the effects of CBD depend on the dose, the strain, the administration time course (acute vs. chronic), and the route of administration. In addition, certain key targets have been related with these CBD pharmacological actions, including cannabinoid receptors (CB1r and CB2r), 5-HT1A receptor and neurogenesis factors.
Preliminary clinical trials also support the efficacy of CBD as an anxiolytic, antipsychotic, and antidepressant, and more importantly, a positive risk-benefit profile. These promising results support the development of large-scale studies to further evaluate CBD as a potential new drug for the treatment of these psychiatric disorders.”
https://pubmed.ncbi.nlm.nih.gov/33228239/
https://www.mdpi.com/2218-273X/10/11/1575

 “Little is known about the patients’ view on treatment with medical cannabis (MC) for Parkinson’s disease (PD).
“Little is known about the patients’ view on treatment with medical cannabis (MC) for Parkinson’s disease (PD). “The COVID-19 pandemic caused by SARS-CoV-2 is a deadly disease afflicting millions. The pandemic continues affecting population due to nonavailability of drugs and vaccines. The pathogenesis and complications of infection mainly involve hyperimmune-inflammatory responses. Thus, therapeutic strategies rely on repurposing of drugs aimed at reducing infectivity and inflammation and modulate immunity favourably.
“The COVID-19 pandemic caused by SARS-CoV-2 is a deadly disease afflicting millions. The pandemic continues affecting population due to nonavailability of drugs and vaccines. The pathogenesis and complications of infection mainly involve hyperimmune-inflammatory responses. Thus, therapeutic strategies rely on repurposing of drugs aimed at reducing infectivity and inflammation and modulate immunity favourably.
 “The increasing legalization of Cannabis for recreational and medicinal purposes in the United States has spurred renewed interest in the therapeutic potential of cannabinoids (CBs) for human disease.
“The increasing legalization of Cannabis for recreational and medicinal purposes in the United States has spurred renewed interest in the therapeutic potential of cannabinoids (CBs) for human disease. “Medical cannabis and individual cannabinoids, such as tetrahydrocannabinol (THC) and cannabidiol (CBD), are receiving growing attention in both the media and the scientific literature. The Cannabis plant, however, produces over 100 different cannabinoids, and cannabigerol (CBG) serves as the precursor molecule for the most abundant phytocannabinoids.
“Medical cannabis and individual cannabinoids, such as tetrahydrocannabinol (THC) and cannabidiol (CBD), are receiving growing attention in both the media and the scientific literature. The Cannabis plant, however, produces over 100 different cannabinoids, and cannabigerol (CBG) serves as the precursor molecule for the most abundant phytocannabinoids. “The endocannabinoid (eCB) system encompasses the eCBs anandamide and 2-arachidonoylglycerol, their anabolic/catabolic enzymes, and the cannabinoid CB1 and CB2 receptors. Its expansion to include several eCB-like lipid mediators, their metabolic enzymes, and their molecular targets, forms the endocannabinoidome (eCBome).
“The endocannabinoid (eCB) system encompasses the eCBs anandamide and 2-arachidonoylglycerol, their anabolic/catabolic enzymes, and the cannabinoid CB1 and CB2 receptors. Its expansion to include several eCB-like lipid mediators, their metabolic enzymes, and their molecular targets, forms the endocannabinoidome (eCBome). “The aberrant accumulation of disease-specific protein aggregates accompanying cognitive decline is a pathological hallmark of age-associated neurological disorders, also termed as proteinopathies, including Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, amyotrophic lateral sclerosis and multiple sclerosis.
“The aberrant accumulation of disease-specific protein aggregates accompanying cognitive decline is a pathological hallmark of age-associated neurological disorders, also termed as proteinopathies, including Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, amyotrophic lateral sclerosis and multiple sclerosis. “Cannabidiol (CBD) is a non-psychoactive phytocannabinoid known for its beneficial effects including antioxidant and anti-inflammatory properties. Moreover, CBD is a compound with antidepressant, anxiolytic, anticonvulsant and antipsychotic effects. Thanks to all these properties, the interest of the scientific community for it has grown.
“Cannabidiol (CBD) is a non-psychoactive phytocannabinoid known for its beneficial effects including antioxidant and anti-inflammatory properties. Moreover, CBD is a compound with antidepressant, anxiolytic, anticonvulsant and antipsychotic effects. Thanks to all these properties, the interest of the scientific community for it has grown. “(E)-β-caryophyllene (BCP) is a bicyclic sesquiterpene widely distributed in the plant kingdom, where it contributes a unique aroma to essential oils and has a pivotal role in the survival and evolution of higher plants.
“(E)-β-caryophyllene (BCP) is a bicyclic sesquiterpene widely distributed in the plant kingdom, where it contributes a unique aroma to essential oils and has a pivotal role in the survival and evolution of higher plants.