 “Marijuana is the dried leaves, stems, and flowers of a 1- to 5-m weed originating from Central Asia. The most common varieties are Cannabis sativa and Cannabis indica. It is usually inhaled as smoke but can also be used as a vapor, taken by mouth as a spray, ingested in tea or as butter in baked goods, or in capsule form and used as an oil. Cannabis has been widely used to treat many medical conditions such as multiple sclerosis symptoms, mood disorders, pain, sleep disorders, and seizures among others. Preclinical and clinical studies have been done over the past decade, among them there are few randomized placebo-controlled trials. In the last few years, Cannabis has been proposed as a potential therapy for patients with drug-resistant epilepsy. This review analyzes the best information about the use of cannabis in adult patients, reviewing aspects of efficacy and safety.”
“Marijuana is the dried leaves, stems, and flowers of a 1- to 5-m weed originating from Central Asia. The most common varieties are Cannabis sativa and Cannabis indica. It is usually inhaled as smoke but can also be used as a vapor, taken by mouth as a spray, ingested in tea or as butter in baked goods, or in capsule form and used as an oil. Cannabis has been widely used to treat many medical conditions such as multiple sclerosis symptoms, mood disorders, pain, sleep disorders, and seizures among others. Preclinical and clinical studies have been done over the past decade, among them there are few randomized placebo-controlled trials. In the last few years, Cannabis has been proposed as a potential therapy for patients with drug-resistant epilepsy. This review analyzes the best information about the use of cannabis in adult patients, reviewing aspects of efficacy and safety.”
https://www.ncbi.nlm.nih.gov/pubmed/31895185
https://insights.ovid.com/crossref?an=00004691-202001000-00003


 “In Italy, medical grade cannabis (MGC) can be prescribed for different medical conditions, including drug-resistant epilepsy (DRE), once standard and approved therapies have failed, or caused non-tolerable side effects.
“In Italy, medical grade cannabis (MGC) can be prescribed for different medical conditions, including drug-resistant epilepsy (DRE), once standard and approved therapies have failed, or caused non-tolerable side effects. “Prostate cancer patients receiving androgen-deprivation therapy (ADT) often experience a combination of disease symptoms and treatment side effects. The therapeutic use of
“Prostate cancer patients receiving androgen-deprivation therapy (ADT) often experience a combination of disease symptoms and treatment side effects. The therapeutic use of  “Parkinson’s disease (PD) and L-DOPA-induced dyskinesia (LID) are motor disorders with significant impact on the patient’s quality of life. Unfortunately, pharmacological treatments that improve these disorders without causing severe side effects are not yet available. Delay in initiating L-DOPA is no longer recommended as LID development is a function of disease duration rather than cumulative L-DOPA exposure.
“Parkinson’s disease (PD) and L-DOPA-induced dyskinesia (LID) are motor disorders with significant impact on the patient’s quality of life. Unfortunately, pharmacological treatments that improve these disorders without causing severe side effects are not yet available. Delay in initiating L-DOPA is no longer recommended as LID development is a function of disease duration rather than cumulative L-DOPA exposure.
 “Muscle pain affects approximately 11-24% of the global population.
“Muscle pain affects approximately 11-24% of the global population. “Indisputably, cancer is a global crisis that requires immediate intervention. Despite the use of conventional treatments over the past decades, it is acceptable to admit that these are expensive, invasive, associated with many side effects and, therefore, a reduced quality of life.
“Indisputably, cancer is a global crisis that requires immediate intervention. Despite the use of conventional treatments over the past decades, it is acceptable to admit that these are expensive, invasive, associated with many side effects and, therefore, a reduced quality of life.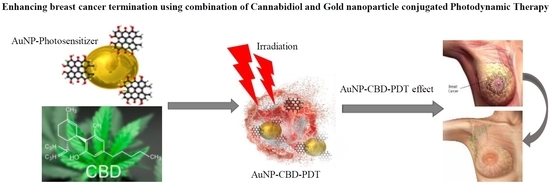
 “The endocannabinoid system (ECS) is a multifunctional homeostatic system involved in many physiological and pathological conditions. The ligands of the ECS are the endocannabinoids, whose actions are mimicked by exogenous cannabinoids, such as phytocannabinoids and synthetic cannabinoids. Responses to the ligands of the ECS are mediated by numerous receptors like the classical cannabinoid receptors (CB1 and CB2) as well as ECS-related receptors, e.g., G protein-coupled receptors 18 and 55 (GPR18 and GPR55), transient receptor potential ion channels, and nuclear peroxisome proliferator-activated receptors. The ECS regulates almost all levels of female reproduction, starting with oocyte production through to parturition. Dysregulation of the ECS is associated with the development of gynecological disorders from fertility disorders to cancer. Cannabinoids that act at the ECS as specific agonists or antagonists may potentially influence dysregulation and, therefore, represent new therapeutic options for the therapy of gynecological disorders.”
“The endocannabinoid system (ECS) is a multifunctional homeostatic system involved in many physiological and pathological conditions. The ligands of the ECS are the endocannabinoids, whose actions are mimicked by exogenous cannabinoids, such as phytocannabinoids and synthetic cannabinoids. Responses to the ligands of the ECS are mediated by numerous receptors like the classical cannabinoid receptors (CB1 and CB2) as well as ECS-related receptors, e.g., G protein-coupled receptors 18 and 55 (GPR18 and GPR55), transient receptor potential ion channels, and nuclear peroxisome proliferator-activated receptors. The ECS regulates almost all levels of female reproduction, starting with oocyte production through to parturition. Dysregulation of the ECS is associated with the development of gynecological disorders from fertility disorders to cancer. Cannabinoids that act at the ECS as specific agonists or antagonists may potentially influence dysregulation and, therefore, represent new therapeutic options for the therapy of gynecological disorders.”