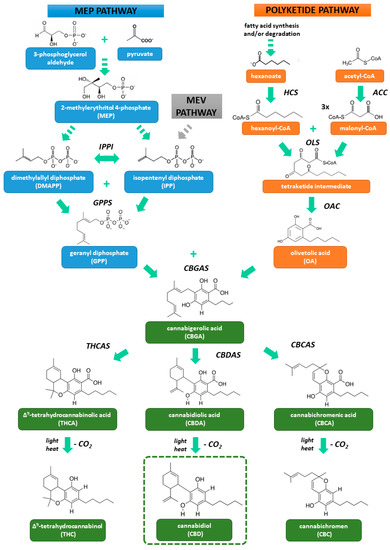
 “Cannabidiol (CBD) is a non-intoxicating and generally well-tolerated constituent of cannabis which exhibits potential beneficial properties in a wide range of diseases, including cardiovascular disorders.
“Cannabidiol (CBD) is a non-intoxicating and generally well-tolerated constituent of cannabis which exhibits potential beneficial properties in a wide range of diseases, including cardiovascular disorders.
Due to its complex mechanism of action, CBD may affect the cardiovascular system in different ways. Thus, we reviewed the influence of CBD on this system in health and disease to determine the potential risk of cardiovascular side effects during CBD use for medical and wellness purposes and to elucidate its therapeutic potential in cardiovascular diseases.
Administration of CBD to healthy volunteers or animals usually does not markedly affect hemodynamic parameters. Although CBD has been found to exhibit vasodilatory and antioxidant properties in hypertension, it has not affected blood pressure in hypertensive animals. Hypotensive action of CBD has been mainly revealed under stress conditions.
Many positive effects of CBD have been observed in experimental models of heart diseases (myocardial infarction, cardiomyopathy, myocarditis), stroke, neonatal hypoxic ischemic encephalopathy, sepsis-related encephalitis, cardiovascular complications of diabetes, and ischemia/reperfusion injures of liver and kidneys.
In these pathological conditions CBD decreased organ damage and dysfunction, oxidative and nitrative stress, inflammatory processes and apoptosis, among others. Nevertheless, further clinical research is needed to recommend the use of CBD in the treatment of cardiovascular diseases.”
https://pubmed.ncbi.nlm.nih.gov/32937917/
https://www.mdpi.com/1422-0067/21/18/6740

 “Anxiety disorders have the highest lifetime prevalence of any mental illness worldwide, leading to high societal costs and economic burden. Current pharmacotherapies for anxiety disorders are associated with adverse effects and low efficacy.
“Anxiety disorders have the highest lifetime prevalence of any mental illness worldwide, leading to high societal costs and economic burden. Current pharmacotherapies for anxiety disorders are associated with adverse effects and low efficacy.
 “Mutations in SYNGAP1 are associated with developmental delay, epilepsy, and autism spectrum disorder (ASD). Epilepsy is often drug-resistant in this syndrome with frequent drop attacks.
“Mutations in SYNGAP1 are associated with developmental delay, epilepsy, and autism spectrum disorder (ASD). Epilepsy is often drug-resistant in this syndrome with frequent drop attacks.

 “Autism spectrum disorder (ASD) is a multifactorial, pervasive neurodevelopmental disorder defined by the core symptoms of significant impairment in social interaction and communication as well as restricted, repetitive patterns of behavior. In addition to these core behaviors, persons with ASD frequently have associated noncore behavioral disturbance (ie, self-injury, aggression), as well as several medical comorbidities. Currently, no effective treatment exists for the core symptoms of ASD.
“Autism spectrum disorder (ASD) is a multifactorial, pervasive neurodevelopmental disorder defined by the core symptoms of significant impairment in social interaction and communication as well as restricted, repetitive patterns of behavior. In addition to these core behaviors, persons with ASD frequently have associated noncore behavioral disturbance (ie, self-injury, aggression), as well as several medical comorbidities. Currently, no effective treatment exists for the core symptoms of ASD. “Non-Uremic Calciphylaxis (NUC) is a rare condition that often manifests as intractable and painful integumentary wounds, afflicting patients with a high burden of co-morbidity.
“Non-Uremic Calciphylaxis (NUC) is a rare condition that often manifests as intractable and painful integumentary wounds, afflicting patients with a high burden of co-morbidity.
 “Cannabidiol (CBD) is considered a non-psychoactive, antioxidant, and anti-inflammatory compound derived from the Cannabis sativa plant.
“Cannabidiol (CBD) is considered a non-psychoactive, antioxidant, and anti-inflammatory compound derived from the Cannabis sativa plant. “Cannabidiol (CBD) is a non-intoxicating phytocannabinoid from cannabis sativa that has demonstrated anti-inflammatory effects in several inflammatory conditions including arthritis.
“Cannabidiol (CBD) is a non-intoxicating phytocannabinoid from cannabis sativa that has demonstrated anti-inflammatory effects in several inflammatory conditions including arthritis.