 “The therapeutic effect of the Cannabis plant largely depends on the presence and specific ratio of a spectrum of phytocannabinoids. While prescription of medicinal Cannabis for various conditions constantly grows, its consumption is mostly limited to oral or respiratory pathways, impeding its duration of action, bioavailability and efficacy. Herein, a long-acting formulation in the form of melt-printed polymeric microdepots for full-spectrum cannabidiol(CBD)-rich extract administration is described. When injected subcutaneously in mice, the microdepots facilitate sustained release of the encapsulated extract over a two-week period. The prolonged delivery results in elevated serum levels of multiple, major and minor, phytocannabinoids for over 14 days, compared to Cannabis extract injection. A direct analysis of the microdepots retrieved from the injection site gives rise to an empirical model for the release kinetics of the phytocannabinoids as a function of their physical traits. As a proof of concept, we compare the long-term efficacy of a single administration of the microdepots to a single administration of Cannabis extract in pentylenetetrazol-induced convulsions model. One week following administration, the microdepots reduce the incidence of tonic-clonic seizures by 40%, increase the survival rate by 50%, and the latency to first tonic-clonic seizures by 170%. These results suggest that a long-term full-spectrum Cannabis delivery system may provide new form of Cannabis administration and treatments.”
“The therapeutic effect of the Cannabis plant largely depends on the presence and specific ratio of a spectrum of phytocannabinoids. While prescription of medicinal Cannabis for various conditions constantly grows, its consumption is mostly limited to oral or respiratory pathways, impeding its duration of action, bioavailability and efficacy. Herein, a long-acting formulation in the form of melt-printed polymeric microdepots for full-spectrum cannabidiol(CBD)-rich extract administration is described. When injected subcutaneously in mice, the microdepots facilitate sustained release of the encapsulated extract over a two-week period. The prolonged delivery results in elevated serum levels of multiple, major and minor, phytocannabinoids for over 14 days, compared to Cannabis extract injection. A direct analysis of the microdepots retrieved from the injection site gives rise to an empirical model for the release kinetics of the phytocannabinoids as a function of their physical traits. As a proof of concept, we compare the long-term efficacy of a single administration of the microdepots to a single administration of Cannabis extract in pentylenetetrazol-induced convulsions model. One week following administration, the microdepots reduce the incidence of tonic-clonic seizures by 40%, increase the survival rate by 50%, and the latency to first tonic-clonic seizures by 170%. These results suggest that a long-term full-spectrum Cannabis delivery system may provide new form of Cannabis administration and treatments.”
Tag Archives: treatment
Two-weeks treatment with cannabidiol improves biophysical and behavioral deficits associated with experimental type-1 diabetes.
 “The prevalence rates of depression and anxiety are at least two times higher in diabetic patients, increasing morbidity and mortality.
“The prevalence rates of depression and anxiety are at least two times higher in diabetic patients, increasing morbidity and mortality.
Cannabidiol (CBD) has been identified as a therapeutic agent viable to treat diverse psychiatric disorders. Thus, this study aimed to investigate the effect of CBD treatment (once a day for 14 days starting two weeks after diabetes induction; at doses of 0, 3, 10 or 30 mg/kg, i.p.) on depression- and anxiety-like behaviors associated with experimental diabetes induced by streptozotocin (60 mg/kg; i.p.) in rats.
Levels of plasma insulin, blood glucose, and weight gain were evaluated in all experimental groups, including a positive control group treated with imipramine. The rats were tested in the modified forced swimming test (mFST) and elevated plus maze (EPM) test. Besides, the levels of serotonin (5-HT), noradrenaline (NA) and dopamine (DA) in two emotion-related brain regions, the prefrontal cortex (PFC) and hippocampus (HIP) were evaluated using high-pressure liquid chromatography.
Our results showed that CBD treatment (only at the higher dose of 30 mg/kg) reduced the exaggerated depressive- and anxiogenic-like behaviors of diabetic (DBT) rats, which may be associated with altered 5-HT, NA and/or DA levels observed in the PFC and HIP. Treatment with CBD (higher dose) also induced a significant increase in weight gain and the insulin levels (and consequently reduced glycemia) in DBT rats. The long-term CBD effects gave rise to novel therapeutic strategies to limit the physiological and neurobehavioral deficits in DBT rats.
This approach provided evidence that CBD can be useful for treating psychiatry comorbidities in diabetic patients.”
https://www.ncbi.nlm.nih.gov/pubmed/32360935
“Treatment of diabetic rats with cannabidiol induced antidepressant- and anxiolytic-like behaviors.”
https://www.sciencedirect.com/science/article/abs/pii/S0304394020302901?via%3Dihub
Altered dopamine D3 receptor gene expression in MAM model of schizophrenia is reversed by peripubertal cannabidiol treatment.
 “Gestational methylazoxymethanol acetate (MAM) treatment produces offspring with adult phenotype relevant to schizophrenia, including positive- and negative-like symptoms, cognitive deficits, dopaminergic dysfunction, structural and functional abnormalities.
“Gestational methylazoxymethanol acetate (MAM) treatment produces offspring with adult phenotype relevant to schizophrenia, including positive- and negative-like symptoms, cognitive deficits, dopaminergic dysfunction, structural and functional abnormalities.
Here we show that adult rats prenatally treated with MAM at gestational day 17 display significant increase in dopamine D3 receptor (D3) mRNA expression in prefrontal cortex (PFC), hippocampus and nucleus accumbens, accompanied by increased expression of dopamine D2 receptor (D2) mRNA exclusively in the PFC. Furthermore, a significant change in the blood perfusion at the level of the circle of Willis and hippocampus, paralleled by the enlargement of lateral ventricles, was also detected by magnetic resonance imaging (MRI) techniques.
Peripubertal treatment with the non-euphoric phytocannabinoid cannabidiol (30 mg/kg) from postnatal day (PND) 19 to PND 39 was able to reverse in MAM exposed rats: i) the up-regulation of the dopamine D3 receptor mRNA (only partially prevented by haloperidol 0.6 mg/kg/day); and ii) the regional blood flow changes in MAM exposed rats. Molecular modelling predicted that cannabidiol could bind preferentially to dopamine D3 receptor, where it may act as a partial agonist according to conformation of ionic-lock, which is higly conserved in GPCRs.
In summary, our results demonstrate that the mRNA expression of both dopamine D2 and D3 receptors is altered in the MAM model; however only the transcript levels of D3 are affected by cannabidiol treatment, likely suggesting that this gene might not only contribute to the schizophrenia symptoms but also represent an unexplored target for the antipsychotic activity of cannabidiol.”
https://www.ncbi.nlm.nih.gov/pubmed/32360362
https://www.sciencedirect.com/science/article/abs/pii/S000629522030232X?via%3Dihub

Cannabidiol and Other Non-Psychoactive Cannabinoids for Prevention and Treatment of Gastrointestinal Disorders: Useful Nutraceuticals?
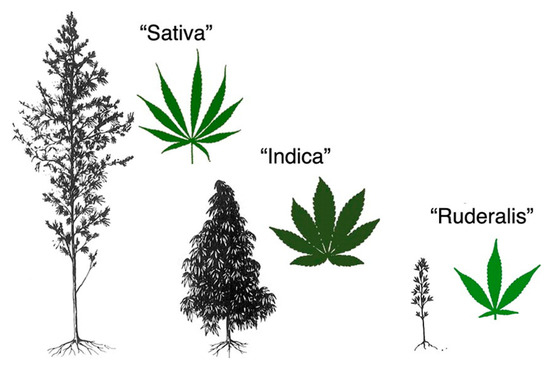
 “Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
“Cannabis sativa is an aromatic annual flowering plant with several botanical varieties, used for different purposes, like the production of fibers, the production of oil from the seeds, and especially for recreational or medical purposes.
Phytocannabinoids (terpenophenolic compounds derived from the plant), include the well-known psychoactive cannabinoid Δ9-tetrahydrocannabinol, and many non-psychoactive cannabinoids, like cannabidiol.
The endocannabinoid system (ECS) comprises of endocannabinoid ligands, enzymes for synthesis and degradation of such ligands, and receptors. This system is widely distributed in the gastrointestinal tract, where phytocannabinoids exert potent effects, particularly under pathological (i.e., inflammatory) conditions.
Herein, we will first look at the hemp plant as a possible source of new functional food ingredients and nutraceuticals that might be eventually useful to treat or even prevent gastrointestinal conditions.
Subsequently, we will briefly describe the ECS and the general pharmacology of phytocannabinoids. Finally, we will revise the available data showing that non-psychoactive phytocannabinoids, particularly cannabidiol, may be useful to treat different disorders and diseases of the gastrointestinal tract.
With the increasing interest in the development of functional foods for a healthy life, the non-psychoactive phytocannabinoids are hoped to find a place as nutraceuticals and food ingredients also for a healthy gastrointestinal tract function.”
https://www.ncbi.nlm.nih.gov/pubmed/32357565
https://www.mdpi.com/1422-0067/21/9/3067
Targeting the Endocannabinoid System in Borderline Personality Disorder.
 “Borderline Personality Disorder (BPD) is a chronic debilitating psychiatric disorder characterized mainly by emotional instability, chaotic interpersonal relationships, cognitive disturbance (e.g. dissociation and suicidal thoughts) and maladaptive behaviors. BPD has a high rate of comorbidity with other mental disorders and high burden on society.
“Borderline Personality Disorder (BPD) is a chronic debilitating psychiatric disorder characterized mainly by emotional instability, chaotic interpersonal relationships, cognitive disturbance (e.g. dissociation and suicidal thoughts) and maladaptive behaviors. BPD has a high rate of comorbidity with other mental disorders and high burden on society.
In this review, we focus on two compromised brain regions in BPD – the hypothalamus and the corticolimbic system, emphasizing the involvement and potential contribution of the endocannabinoid system (ECS) to improvement in symptoms and coping.
The hypothalamus-regulated endocrine axes (hypothalamic pituitary – gonadal, thyroid & adrenal) have been found to be dysregulated in BPD. There is also substantial evidence for limbic system structural and functional changes in BPD, especially in amygdala and hippocampus, including cortical regions within the corticolimbic system.
Extensive expression of CB1 and CB2 receptors of the ECS has been found in limbic regions and the hypothalamus. This opens new windows of opportunity for treatment with cannabinoids such as cannabidiol (CBD) as no other pharmacological treatment has shown long-lasting improvement in the BPD population to date.
This review aims to show the potential role of the ECS in BPD patients through their most affected brain regions, the hypothalamus and the corticolimbic system. The literature reviewed does not allow for general indications of treatment with CBD in BPD. However, there is enough knowledge to indicate a treatment ratio of high level of CBD to low level of THC.
A randomized controlled trial investigating the efficacy of cannabinoid based treatments in BPD is warranted.”
Potential therapeutic treatments of cancer-induced bone pain.
 “The treatment of cancer-induced bone pain (CIBP) has been proven ineffective and relies heavily on opioids, the target of highly visible criticism for their negative side effects.
“The treatment of cancer-induced bone pain (CIBP) has been proven ineffective and relies heavily on opioids, the target of highly visible criticism for their negative side effects.
Alternative therapeutic agents are needed and the last few years have brought promising results, detailed in this review.
RECENT FINDINGS:
Cysteine/glutamate antiporter system, xc, cannabinoids, kappa opioids, and a ceramide axis have all been shown to have potential as novel therapeutic targets without the negative effects of opioids.
SUMMARY:
Review of the most recent and promising studies involving CIBP, specifically within murine models. Cancer pain has been reported by 30-50% of all cancer patients and even more in late stages, however the standard of care is not effective to treat CIBP. The complicated and chronic nature of this type of pain response renders over the counter analgesics and opioids largely ineffective as well as difficult to use due to unwanted side effects. Preclinical studies have been standardized and replicated while novel treatments have been explored utilizing various alternative receptor pathways: cysteine/glutamate antiporter system, xc, cannabinoid type 1 receptor, kappa opioids, and a ceramide axis sphingosine-1-phosphate/sphingosine-1-phosphate receptor 1.”
https://www.ncbi.nlm.nih.gov/pubmed/32349095
Innovative methods for the preparation of medical Cannabis oils with a high content of both cannabinoids and terpenes.
 “Cannabis-based medications are being increasingly used for the treatment of different clinical conditions.
“Cannabis-based medications are being increasingly used for the treatment of different clinical conditions.
Among all galenic formulations, olive oil extracts from medical Cannabis are the most prescribed ones for their easy preparation and usage. A great variety of methods have been described so far for the extraction of medical Cannabis oils to reach a high yield of Δ9-tetrahydrocannabinol (Δ9-THC), but poor attention has been paid to the preservation of the terpene fraction from the plant, which may contribute to the overall bioactivity of the extracts.
In this context, the present study was aimed at the chemical characterization of different medical Cannabis oils prepared by following both innovative and existing extraction protocols, with particular attention to cannabinoids and terpenes, in order to set up a suitable method to obtain an extract rich in these chemical classes. In particular, six different extraction procedures were followed, based on different techniques, of which all but one included a decarboxylation of the plant material.
The profile of cannabinoids was studied in detail by means of HPLC-ESI-MS/MS, while terpenes were characterized by means both GC-MS and GC-FID techniques coupled with solid-phase microextraction operated in the head-space mode (HS-SPME). An innovative method that is based on the extraction of the oil by dynamic maceration at room temperature from plant inflorescences, which were partially decarboxylated in a closed system at a moderate temperature and partially pre-extracted with ethanol, produced similar yields of bioactive compounds as that obtained by using a microwave-assisted distillation of the essential oil from the plant material, in combination with a maceration extraction of the oil from the residue.
Both these new methods provided a higher efficiency over already existing extraction procedures of medical Cannabis oils and they can be applied to obtain a product with a high therapeutic value.”
https://www.ncbi.nlm.nih.gov/pubmed/32334134
“New methods were developed for the extraction of medical Cannabis oils.”
https://www.sciencedirect.com/science/article/abs/pii/S0731708520303897?via%3Dihub
Cannabis and cannabinoids in cancer pain management.
 “An increasing number of patients are turning to cannabis and cannabinoids for management of their palliative and nonpalliative cancer pain and other cancer-related symptoms.
“An increasing number of patients are turning to cannabis and cannabinoids for management of their palliative and nonpalliative cancer pain and other cancer-related symptoms.
Canadians have a legal framework for access to medical cannabis, which provides a unique perspective in a setting lacking robust clinical evidence. This review seeks to delineate the role of cannabis and cannabinoids in cancer pain management and offers insight into the Canadian practice.
RECENT FINDINGS:
A cohort study using nabiximols on advanced cancer pain in patients already optimized on opioids, over 3 weeks, demonstrated improved average pain score. A large observational study of cancer patients using cannabis over 6 months demonstrated a decreased number of patients with severe pain and decreased opioid use, whereas the number of patients reporting good quality of life increased.
SUMMARY:
Good preclinical animal data and a large body of observational evidence point to the potential efficacy of cannabinoids for cancer pain management. However, there are relatively weak data pointing to clinical efficacy from clinical trial data to date. In Canada, the burgeoning cannabis industry has driven the population to embrace a medicine before clinical evidence. There remains a need for high-quality randomized controlled trials to properly assess the effectiveness and safety of medical cannabis, compared with placebo and standard treatments for cancer-related symptoms.”
https://www.ncbi.nlm.nih.gov/pubmed/32332209
https://journals.lww.com/pages/results.aspx?txtKeywords=10.1097%2fSPC.0000000000000493
CBD modulates DNA methylation in mice prefrontal cortex and hippocampus of mice exposed to forced swim.
 “Cannabidiol (CBD), a non-psychotomimetic component of Cannabis sativa plant, shows therapeutic potential in psychiatric disorders, including depression.
“Cannabidiol (CBD), a non-psychotomimetic component of Cannabis sativa plant, shows therapeutic potential in psychiatric disorders, including depression.
The molecular mechanisms underlying the antidepressant-like effects of CBD are not yet understood. Previous studies in differentiated skin cells demonstrated that CBD regulates DNA methylation, an overall repressive epigenetic mechanism. Both stress exposure and antidepressant treatment can modulate DNA methylation in the brain, and lead to gene expression changes associated with depression neurobiology.
We investigated herein if the antidepressant effect of CBD could be associated with changes in DNA methylation in the prefrontal cortex (PFC) and hippocampus (HPC) of mice submitted to the forced swimming test (FST).
Altogether, our results indicate that CBD regulates DNA methylation in brain regions relevant for depression neurobiology, suggesting that this mechanism could be related to CBD-induced antidepressant effects.”
https://www.ncbi.nlm.nih.gov/pubmed/32348868
“Cannabidiol (CBD) shows antidepressant-like properties in mice.”
https://www.sciencedirect.com/science/article/pii/S0166432820303260?via%3Dihub
A randomized, double-blind, placebo-controlled study of daily cannabidiol for the treatment of canine osteoarthritis pain.
 “Over the last two decades, affirmative diagnoses of osteoarthritis in the United States have tripled due to increasing rates of obesity and an aging population.
“Over the last two decades, affirmative diagnoses of osteoarthritis in the United States have tripled due to increasing rates of obesity and an aging population.
Hemp-derived cannabidiol (CBD) is the major non-THC component of cannabis and has been promoted as a potential treatment for a wide variety of disparate inflammatory conditions.
Here we evaluated CBD for its ability to modulate the production of pro-inflammatory cytokines in vitro and in murine models of induced inflammation and further validated the ability of a liposomal formulation to increase bioavailability in mice and in humans.
Subsequently, the therapeutic potential of both naked and liposomally-encapsulated CBD was explored in a 4-week, randomized placebo-controlled, double-blinded study in a spontaneous canine model of osteoarthritis.
In vitro and in mouse models, CBD significantly attenuated the production of pro-inflammatory cytokines IL-6 and TNF-α while elevating levels of anti-inflammatory IL-10. In the veterinary study, CBD significantly decreased pain and increased mobility in a dose-dependent fashion among animals with an affirmative diagnosis of osteoarthritis.
Liposomal CBD (20 mg/day) was as effective as the highest dose of non-liposomal CBD (50 mg/day) in improving clinical outcomes. Hematocrit, comprehensive metabolic profile, and clinical chemistry indicated no significant detrimental impact of CBD administration over the four-week analysis period.
This study supports the safety and therapeutic potential of hemp-derived CBD for relieving arthritic pain and suggests follow-up investigations in humans is warranted.”
